مقالة علمية للدكتور محمد فارس جعباز بعنوان ( Oral Inflammation and Respiratory Diseases )
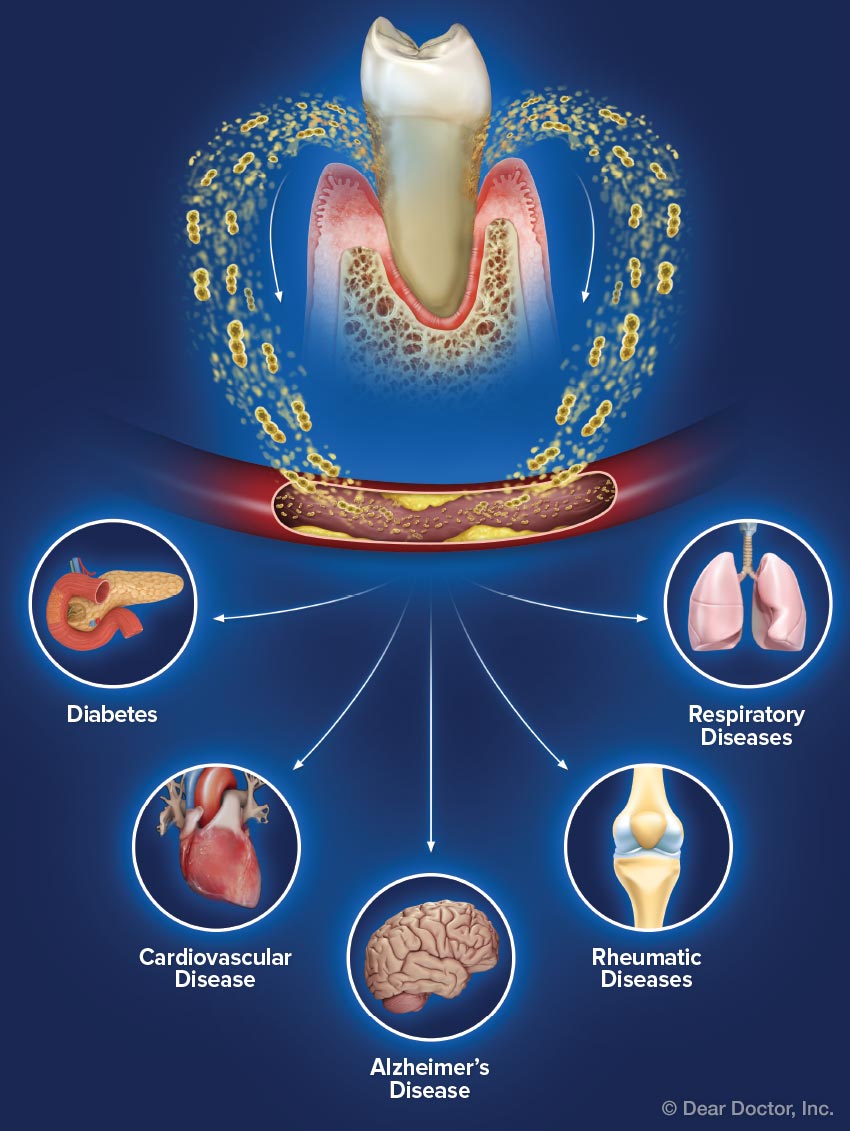
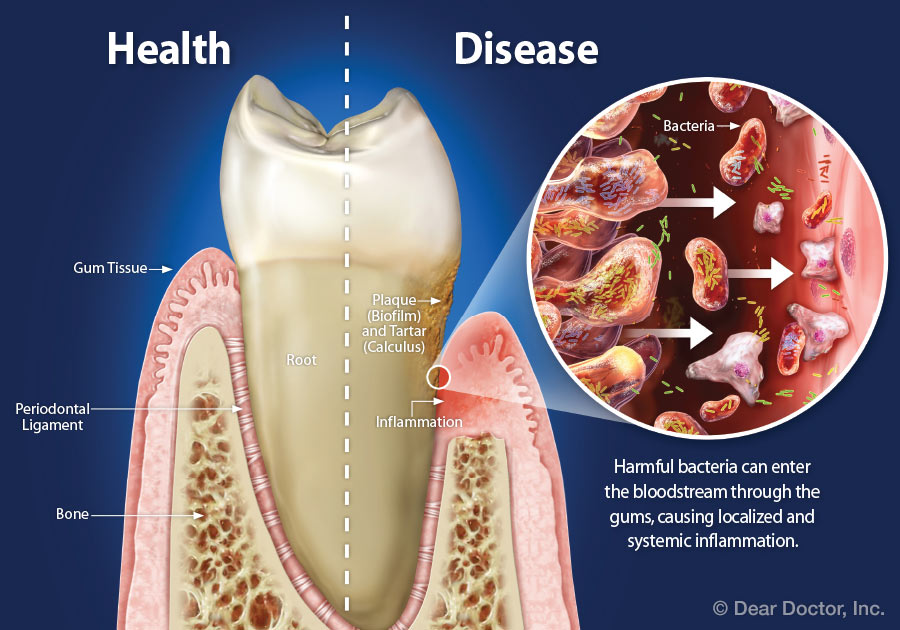
Periodontal disease has been linked to an increased risk of respiratory diseases, such as pneumonia and chronic obstructive pulmonary disease (COPD). We will be briefly describes evidence for this association, and the mechanisms by which oral bacteria may promote colonization of the lungs by pathogens.<br />Pneumonia<br />Pneumonia is defined as inflammation of the lungs resulting from infection, usually bacterial or viral. Pneumonia cases can be divided into two major types: community-acquired and hospital-acquired (nosocomial). About 1.1 million cases of community-acquired pneumonia require hospitalization annually in the United States, with a mortality in hospitalized patients of 12%.1 Bacteria that often colonize the oropharynx and upper airway, such as Streptococcus pneumoniae, Haemophilus influenzae and Mycoplasma pneumoniae, usually cause community-acquired pneumonia.<br /> Nosocomial pneumonia represents 13-18% of hospital-acquired infections and occurs in 0.4-0.7% of hospitalizations; mortality is about 30%.3 Nosocomial pneumonia is usually caused by bacteria acquired from the environment, such as Pseudomonas aeruginosa, Staphylococcus aureus and enteric Gram-negative bacteria.<br /><br />Association Between Oral Bacteria and Pneumonia<br />Several lines of evidence indicate that people with poor oral health are at higher risk for nosocomial pneumonia. First, a number of oral health factors increase the risk of pneumonia, including having teeth or dentures (versus being edentulous without wearing dentures), being dependent on others for oral care (which leads to higher amounts of plaque), and infrequent tooth brushing.<br />Second, microbiological studies reveal a direct association between pneumonia risk and colonization of the teeth and oral cavity by enteric Gram-negative bacteria and respiratory pathogens in intensive care patients.<br />Third, in controlled clinical trials, interventions that inhibited dental plaque, such as treatment with oral or topical antibiotics, chlorhexidine, or povidone-iodine plus tooth brushing, reduced the risk of pneumonia .When data from the five trials in the Table were combined in a meta-analysis.The variety of interventions that reduce respiratory disease suggests that other antibacterial treatments could have similar effects. The antibacterial Colgate® Total® Toothpaste, for example, uses a copolymer to improve retention of the bactericide triclosan on oral surfaces, providing 12-hour antibacterial action and direct inhibition of potent inflammatory mediators.Although its effects on respiratory disease have not been tested, this dentifrice may provide protection because it reduces the growth of oral bacteria and formation of plaque.<br />The association between oral bacteria and pneumonia has implications for the institutionalized, including those living in nursing homes or hospitals for extended periods of time. People in these situations have a higher exposure to pathogens, are less likely to pay close attention to oral health, and are more likely to have poor general health. In descriptive studies, institutionalized subjects have more dental plaque and are more prone to colonization by respiratory pathogens than controls. Therefore, institutionalized people represent a high-risk group for pneumonia related to oral bacteria.<br />Chronic Obstructive Pulmonary Disease<br />Chronic obstructive pulmonary disease (COPD) was the sixth leading cause of death worldwide in 1990.11COPD includes chronic bronchitis, in which irritation of the bronchial airway causes increased mucous production and persistent cough, and emphysema, in which dilation of small air passages leads to lung damage.10<br />Risk factors for COPD include smoking, chronic exposure to atmospheric pollutants, such as second-hand smoke, and genetic conditions.10 COPD patients experience periodic exacerbations for unknown reasons, and bacterial infections caused by H. influenzae, S. pneumoniae, and Moraxella catarrhalis may contribute to these episodes.<br />