تم نشر مقالة علمية للتدريسي في قسم تقنيات التخدير المدرس المساعد علي جليل عسر بعنوانProtective personal equipment and corona viruses
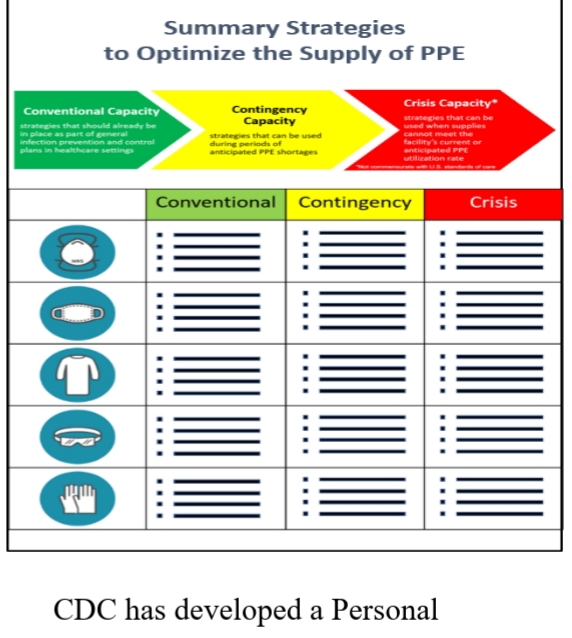
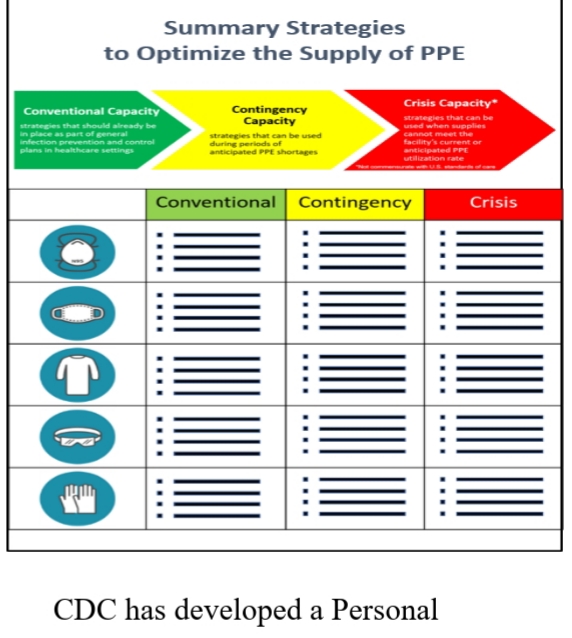
Ali Jalil <br /><br />Protective personal equipment and corona viruses<br /> <br /> Measures for protecting workers from exposure to, and infection with, SARS-CoV-2, the virus that causes Coronavirus Disease 2019 (COVID-19), depend on the type of work being performed and exposure risk, including potential for interaction with people with suspected or confirmed COVID-19 and contamination of the work environment. Employers should adapt infection control strategies based on a thorough hazard assessment, using appropriate combinations of engineering and administrative controls, safe work practices, and personal protective equipment (PPE) to prevent worker exposures. Some OSHA standards that apply to preventing occupational exposure to SARS-CoV-2 also require employers to train workers on elements of infection prevention, including PPE.<br /> Personal protective equipment (PPE) is used every day by healthcare personnel (HCP) to protect themselves, patients, and others when providing care. PPE helps protect HCP from many hazards encountered in healthcare facilities.<br /> The greatly increased need for PPE caused by the COVID-19 pandemic has caused PPE shortages, posing a tremendous challenge to the healthcare system. Healthcare facilities are having difficulty accessing the needed PPE and are having to identify alternate ways to provide patient care.<br />practices.<br /> <br /> CDC has developed a Personal Protective Equipment (PPE) Burn Rate Calculator. Three general strata have been used to describe surge capacity and can be used to prioritize measures to conserve PPE supplies along the continuum of care.<br />Illustration: Strategies to optimize the supplies of PPE<br />Conventional capacity: measures consisting of engineering, administrative, and PPE controls that should already be implemented in general infection prevention and control plans in healthcare settings.<br />Contingency capacity: measures that may be used temporarily during periods of anticipated PPE shortages. Contingency capacity strategies should only be implemented after considering and implementing conventional capacity strategies. While current supply may meet the facility’s current or anticipated utilization rate, there may be uncertainty if future supply will be adequate and, therefore, contingency capacity strategies may be needed.<br />Crisis capacity: strategies that are not commensurate with U.S. standards of care but may need to be considered during periods of known PPE shortages. Crisis capacity strategies should only be implemented after considering and implementing conventional and contingency capacity strategies. Facilities can consider crisis capacity strategies when the supply is not able to meet the facility’s current or anticipated utilization rate.<br /> CDC’s optimization strategies for PPE offer a continuum of options for use when PPE supplies are stressed, running low, or exhausted. Contingency and then crisis capacity measures augment conventional capacity measures and are meant to be considered and implemented sequentially. As PPE availability returns to normal, healthcare facilities should promptly resume standard<br /> <br />