تم نشر مقالة علمية للتدريسي في قسم تقنيات التخدير المدرس المساعد محمد عبد الزهرة صعصاع بعنوان Ultrasound-guided brachial plexus blocks in pediatric anesthesia
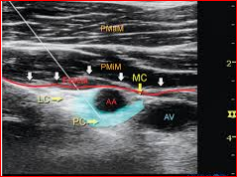
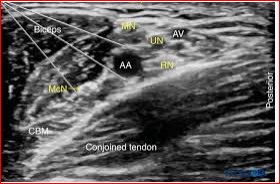
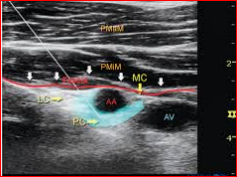
Ultrasound-guided brachial plexus blocks in pediatric anesthesia: non-systematic review<br /><br />Majid Fakhir alhamaidah*1,2, Hussein Ali Hussein 2,3, Hussein alkhfaji 2,4, Sami Raheem Hasan2, Mohammed AbdulZahra and Sasaa5Ali B. Roomi6 <br /> AL-Rifaei General Hospital, Iraq. <br />2 Department of Anesthesia, College of Health and Medical Technology, Al-Ayen University, Iraq<br />3 Nasiriya heart center<br />4 Bent AL Huda hospital, Iraq.<br />5 AL-Mustaqbal university college, department of anesthesia Babel, Iraq <br />6 College of Health and Medical Technology, Al-Ayen University, Iraq. <br />Abstract <br />Background: The ultrasound guidance for regional anesthesia has gate a widespread as a recent technique to identify, visualize, and monitoring targeted nerves, needle insertion, local anesthetic injection and distribution, catheters and adjacent anatomical structures, and helps to avoid complications such as inadvertent intravascular or intrafascicular injection in comparison to other traditional techniques.<br />Purpose of review: To show and explain if any superiority has added to brachial plexus approaches with this sonography guidance for the pediatric population over other traditional techniques in terms of increasing the success rate or reducing the complications.<br />Methods: Three authors independently searched the literature using MEDLINE and EMBASE bibliographic databases, Cochrane Central Register of Controlled Trials (CENTRAL), and manually in either the title or abstract, we also searched Google Scholar, Web of Science and reviewed the references of included trials for potentially relevant trials.<br />Results: Reviewed literature suggests that ultrasound-guided peripheral blocks reduce block performance time in comparison with nerve stimulation, increase the success rate, reduced intended LA agent, and increase the quality of the block (as measured by analgesic consumption, block duration, and pain scores). <br />Conclusion: The introduction of ultrasound imaging improved the safety profile, reduced performance time, and advanced the upper limbs block approach.<br /><br />Keywords: Ultrasound, regional block, brachial plexus, upper limb, upper extremities, pediatric anesthesia. <br /><br />Introduction <br /> Ultrasonography represents a real-time nerve visualization and drug deposition around it, other internal structures including vessels, needle, and catheter became possible to be visualized by this technique. However, its application needs some basic skills (1). Pediatric patients are unlike adults in their anatomical and physiological features, and the landmark technique is not reliable in all patients due to the variability in the age and size (2). With the advancement in sonographic technology, the success rate of blocks has increased and the recommended dose gate less than with other traditional methods for pediatric regional blocks for upper extremities with the assistance of high-frequency transducers (2). There is a tight area around nerves and plexuses in the pediatric group, which is unique to this population that gives better block under ultrasound probe. The pediatric group is not a homogenous population, but they range from neonate to an adolescent and follow to that the depth of nerves and plexuses varies with the age ranging (2).<br />Recently searched published articles showed significant advantages in the field of pediatric anesthesia of the upper limbs, involve the faster sensory and motor blockade and extended duration of sensory blockade compared with using nerve stimulation alone in children (3). Ultrasound-guided upper-extremity peripheral nerve blocks (e.g. axillary, infraclavicular, interscalene, supraclavicular) in children can be performed successfully and safely with a recommended LA dose(4). In addition to reducing the muscle contraction pain that is associated with nerve stimulation with the feasibility and efficiency of ambulatory peripheral nerve catheters in pediatrics (5). <br />Methods<br /> In this review, we searched the current literature available on MEDLINE, EMBASE, and Cochrane Evidence-Based Medicine Reviews. Furthermore, citation reviews and manual search of new journals related to pediatric anesthesia or surgery were done. We included all parallel randomized controlled trials that evaluated the effect of ultrasound guidance to perform a regional blockade technique in children. Comparative studies, question studies, case series, systematic and non-systematic reviews including one or more approaches for brachial plexus blocks were searched. Searching was limited to English language and full-text articles. Four authors read all selected articles independently and a consensus was achieved. The keywords used, alone and in combination were: ultrasound, regional block, regional anesthesia, pediatric anesthesia. A further search of older literature was deemed unsuitable, and ultrasound guidance has only become a usable modality in the last few years. The goal was to review studies about regional anesthesia in pediatrics with peripheral nerve block techniques by comparing ultrasound-guided peripheral nerve block of the upper extremities either alone or by combination with at least one other technique of nerve identification such as; anatomical landmark, paresthesia, or using of a nerve stimulator. <br /><br />Technical Consideration for Pediatrics<br /> Since body water percentage is higher with pediatrics, the identification of body structures like neurons, plexuses is better than adults under the ultrasound guidance, furthermore, bony structures have less ossification making a good quality image. Nerves, plexuses, and other structures in infants and young children are located superficially and could easy visualized by the ultrasound probe. A proper instrument to patient size and age should be available for that. Suitable needle size is needed to avoid nerve injury, and good quality transducer to gate suitable resolution for superficial structures should be prepared (2).<br />Brachial plexus block<br /> The innervation of upper extremities is derived from the brachial plexus which is composed of the union of the cervical roots from C1 to C8 and part from the T1. The main anatomical differences between pediatrics and adult populations, which increase the risk of regional lock during needle insertion with perisubclavian approaches, that the superior part of the lung and apical pleura enter the neck, above the superior thoracic aperture making the risk of plural invasion bigger than with the adults. New ultrasound technology reduced these complications by offering direct and real-time visualization of the needle and any adjacent structures with supraclavicular and infraclavicular approaches.<br /> Brachial plexus block may be achieved at several sites, the appropriateness of each block is determined by the location of the surgery, the ability to properly position the patient, and assessment of pre-existing patient morbidities. The advancement in ultrasound application techniques gave the confidence for aesthesia practitioners to approach the more proximal brachial plexus even in infants and young children, instead of the axillary site which has previously been a preferred location of brachial plexus block in pediatrics (6).<br />Since the innervation of the medial aspect of the proximal arm been separately by the intercostal brachial nerve, the brachial plexus blockade will not provide anesthesia for this area. The clinical significance of this nerve is apparent when a tourniquet is applied to the proximal arm. A transverse subcutaneous field block just below the axilla will achieve anesthesia in this region.<br />Ultrasound Guided Interscalene brachial plexus block<br /> This approach is mainly used to provide anesthesia and analgesia to the shoulder girdle and arm above the elbow, which makes interscalene approach useful for shoulder and even clavicular surgery, but generally it is inappropriate for surgery below the elbow.<br /><br /> The Interscalene block wasn’t very common in the pediatric group because of the potential adverse effects associated with this approach such as pneumothorax, intrathecal injection, and inadvertent injection into a vertebral artery. Also, this technique preferably needs to be performed by an anesthesiologist expert in nerve block. The introduction of ultrasound into clinical practice has markedly increased the use of this approach in clinical practice (7).<br /> The sensitivity of structures close to the interscalene brachial plexus makes precise needle placement imperative mandating the use of ultrasound in younger patients. In comparison with an awake adult patient and anesthetized child, there is no difference in safety issues between the two groups with interscalene approach (7). The ideal position for a child in a supine position with the arms extended alongside the thorax and the head slightly turned to the contralateral side (2).<br />Ultrasound Guided Supraclavicular Approach<br /> Supraclavicular route of brachial plexus block is extremely recommended for pediatric patients to allowing real-time visualization of the needle tip and lung parenchyma at this level, Ultrasound technique increased the safety profile of this approach, so it can be considered as ‘The Spinal of Arm’, in which local anaesthetic agent is delivered at a point where the three trunks are compactly arranged and carry entire sensory, motor and sympathetic innervations of the upper extremity (8). With the assistance of ultrasound technique, there was short time performance, less number of needle insertions, a smaller volume of the intended local anaesthetic agent, rapid onset of action, higher success rate and less complications (9). Supraclavicular approaches are indicated for the surgical procedures on the shoulder or the proximal part of the arm, forearm and the hand.<br />Ultrasound Guided Infraclavicular Approach<br /> The infraclavicular block is a brachial plexus block used as an alternative or adjunct to general anesthesia. It can be used for postoperative pain control for upper extremity surgeries by blocking the divisions or the cords of the brachial plexus, making the operations for elbow, forearm, and hand possible (8). Marhofer et al. (10) presented that infraclavicular brachial plexus blocks with Ultrasound guidance offer sensory and motor responses faster than with nerve stimulation, and longer time of sensory blockade in pediatric patients (11).<br />Ultrasound Guided Axillary Approach<br /> The axillary brachial plexus block can be used to provide reliable anesthesia and analgesia to the arm distal to the shoulder, including Surgery of the elbow, forearm, and hand; closed reduction of fractures of the elbow, forearm, and hand for postreduction pain relief. <br /> Recent Literature reviews showed that the axillary block is the most common, easiest and safest method in pediatric patients, with the goal of blocking the terminal branches of the brachial plexus. It has the least complications when compared with the other blocks for the upper limb. Inadvertent arterial puncture and intraneural injection are the most undesirable feared complication. It is usually thought intraneural injection is the main cause of permanent nerve damage and mostly undetected in the patient under general anesthesia. (11)<br />Ultrasound Guide for Elbow and Forearm<br /> Brachial plexus blocks by elbow and forearm approaches are not so common approaches in pediatrics but usually induced as supporting methods for partially failed brachial blocks. Ultrasound technology extends the indications of these approaches. Median and ulnar nerves are located superficially and can be blocked easily at any point of their way from the wrist to the axilla, but the operator should be carefully oriented to differentiate between the nerves and the tendons at the level of the wrist since they have similar view under ultrasound probe1. A complete block can be gain with a small volume of local anesthetic agents. (11)<br />Conclusion <br /> Depending on the outcomes gained from the reviewed studies and materials, the authors concluded with consent that ultrasound guidance increases the success rate for brachial plexus blocks applied to pediatric patients. These studies showed decreased performance time, good visualization of the needles, catheters, adjacent anatomical structures, and local anesthetic distribution. With the assistance of ultrasound guidance, the inadvertent blood vessel punctures were significantly reduced. (12). The use of ultrasonography to guide the peripheral nerve blocks in the pediatric population made these procedures safer, either alone or in concomitant with the traditional techniques. (13,14), ultrasound guidance facilitated the catheter placement for continuous nerve blocks (12) and induced less intraoperative consumption of opioids compared with other techniques (15) Less volume of local anesthetic was sufficient to perform the block (15). Similar block success, postoperative sensory block durations, and pain scores could be obtained during infraclavicular brachial plexus in pediatric patients with lower local anesthetic volumes (16). Recently reviewed studies showed that the ultrasound technique has grown to be the standard for peripheral analgesia and pain control (17).<br />References<br />1. Ilfeld BM, Wright TW, Enneking KF, Morey TE. Joint range of motion after total shoulder arthroplasty with and without a continuous interscalene nerve block: a retrospective, case-control study. Regional Anesthesia & Pain Medicine. 2005;30(5):429-33.<br />2. Delvi MB. Ultrasound-guided peripheral and truncal blocks in pediatric patients. Saudi journal of anaesthesia. 2011;5(2):208.<br />3. Tsui BC, Suresh S. Ultrasound imaging for regional anesthesia in infants, children, and adolescentsa review of current literature and its application in the practice of extremity and trunk blocks. Anesthesiology: The Journal of the American Society of Anesthesiologists. 2010;112(2):473-92.<br />4. Suresh S, Ecoffey C, Bosenberg A, Lonnqvist P-A, De Oliveira GS, de Leon Casasola O, et al. The European Society of regional anaesthesia and pain Therapy/American Society of regional anesthesia and Pain medicine recommendations on local anesthetics and adjuvants dosage in pediatric regional anesthesia. Reg Anesth Pain Med. 2018;43(2):211-6.<br />5. Perlas A, Lobo G, Lo N, Brull R, Chan VW, Karkhanis R. Ultrasound-guided supraclavicular block: outcome of 510 consecutive cases. Regional Anesthesia & Pain Medicine. 2009;34(2):171-6--6.<br />6. Veneziano G, Betran R, Bhalla T. Peripheral regional anesthesia in infants and children: an update. Anaesthesia, Pain & Intensive Care. 2019:267-73.<br />7. Taenzer A, Walker BJ, Bosenberg AT, Krane EJ, Martin LD, Polaner DM, et al. Interscalene Brachial Plexus Blocks Under General Anesthesia in Children: Is This Safe Practice? Reg Anesth Pain Med. 2014;39(6):502-5.<br />8. Ríos-Medina AM, Caicedo-Salazar J, Vásquez-Sadder MI, Aguirre-Ospina OD, González MP. Regional anesthesia in pediatrics–Non-systematic literature review. Colombian Journal of Anesthesiology. 2015;43(3):204-13.<br />9. Amiri HR, Espandar R. Upper extremity surgery in younger children under ultrasound-guided supraclavicular brachial plexus block: a case series. Journal of children's orthopaedics. 2011;5(1):5-9.<br />10. Marhofer P, Sitzwohl C, Greher M, Kapral S. Ultrasound guidance for infraclavicular brachial plexus anaesthesia in children. Anaesthesia. 2004;59(7):642-6.<br />11. Dalens B. Regional anesthesia in children. Anesthesia & Analgesia. 1989;68(5):654-72.<br />12. Guay J, Suresh S, Kopp S. The use of ultrasound guidance for perioperative neuraxial and peripheral nerve blocks in children. Cochrane Database of Systematic Reviews. 2019(2).<br />13. Krodel DJ, Marcelino R, Sawardekar A, Suresh S. Pediatric regional anesthesia: A review and Update. Current Anesthesiology Reports. 2017;7(2):227-37.<br />14. Frenkel O, Liebmann O, Fischer JW. Ultrasound-guided forearm nerve blocks in kids: a novel method for pain control in the treatment of hand-injured pediatric patients in the emergency department. Pediatric emergency care. 2015;31(4):255-9.<br />15. Lam DK, Corry GN, Tsui BC. Evidence for the use of ultrasound imaging in pediatric regional anesthesia: a systematic review. 2016.<br />16. Ince I, Aksoy M, Dostbil A, Tuncer K. Can we use lower volume of local anesthetic for infraclavicular brachial plexus nerve block under ultrasound guidance in children? Journal of clinical anesthesia. 2017;41:132-6.<br />17. Yayık AM, Ekinci M, Gölboyu BE, Ergüney ÖD, Çelikkaya ME, Ahıskalıoğlu EO, et al. Pediyatrik inguinal herni tamirinde ultrasonografi eşliğinde yapılan transversus abdominis plan bloğu ile yara yeri infiltrasyonunun karşılaştırılması: Randomize klinik çalışma. 2017.<br /><br />