م.م.دعاء ساهي حسونHistology, Salivary Glands
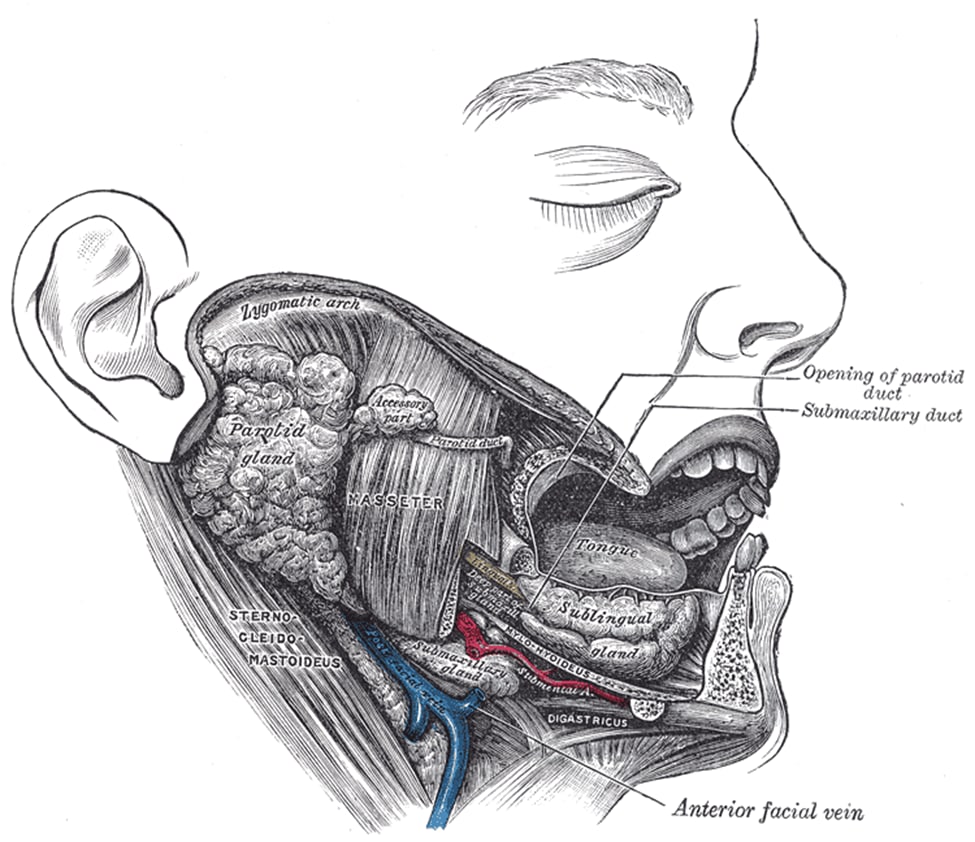
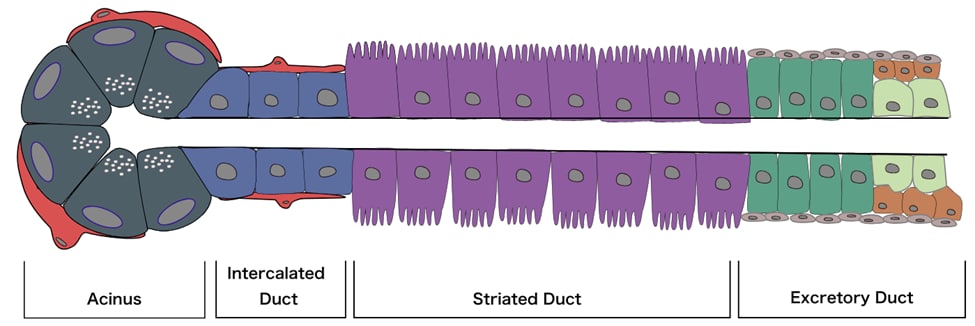
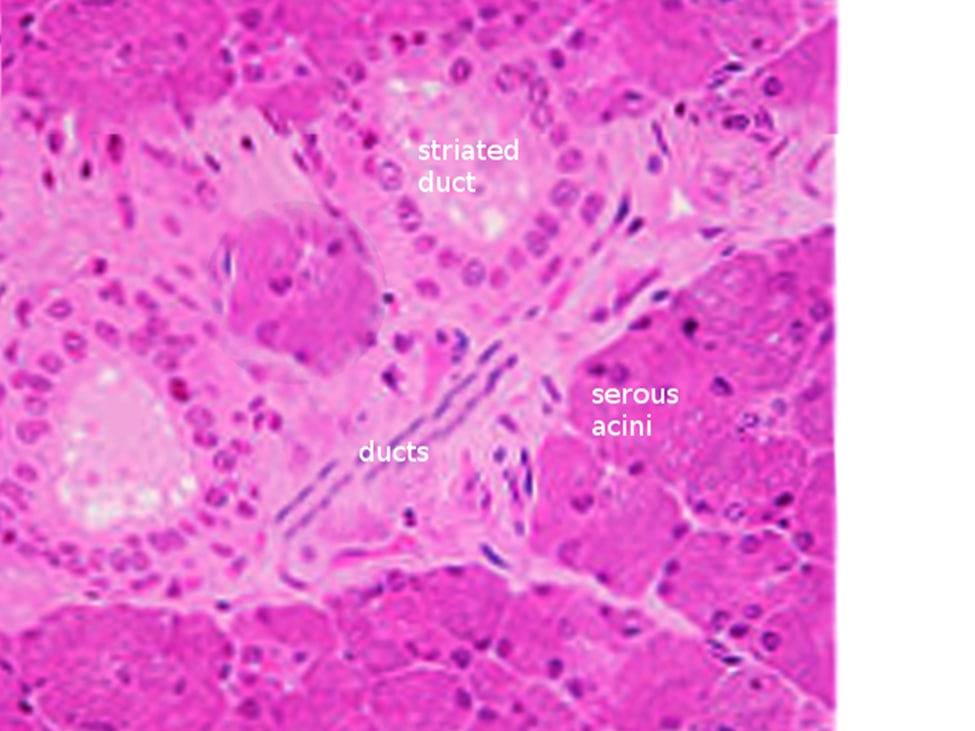
Humans possess three pairs of major salivary glands and approximately 600 to 1000 minor glands. The major salivary glands are the submandibular gland (SMG), sublingual gland (SLG), and the parotid gland (PG). Of these, the parotid gland is the largest and most important in terms of salivary production, providing approximately 50% of the total saliva volume. Collectively, all the major salivary glands function to secrete saliva, which contains a host of electrolytes, such as bicarbonate, and enzymes, such as salivary amylase, which break down carbohydrates in the oral cavity<br /><br />Structure<br />The major salivary glands have essentially the same structure: secretory end-pieces termed acini that produce saliva, which flows into arborized ducts that open into the oral cavity. All salivary glands are encapsulated and divided into divisions called lobes, which further subdivide into lobules, each of which is separated by a connective tissue septum. Each salivary gland is made up of two separate parts: a serous portion, responsible for secreting watery saliva, and a mucous portion, responsible for a more viscous fluid. The three major salivary glands are all composed of a mixture of these two types of cells. The parotid gland is composed primarily of serous acini and produces watery saliva, which lubricates the oral cavity and helps with swallowing, talking, and maintaining homeostasis. The submandibular gland has a predominance of serous cells with some mucous cells. The sublingual gland is composed of mostly mucous acini and thus produces the thickest and most viscous saliva. Both parasympathetic and sympathetic branches of the autonomic nervous system stimulate the secretion of saliva via aquaporins, specifically aquaporin 1 and 5. Electrolytes that will ultimately get released in saliva are first secreted from the acini through the intercalated ducts, into the striated ducts where they are moved out into the lumen through each gland’s respective duct via transmembrane active pumping.<br /><br /><br />Function<br />As previously mentioned, all three major salivary glands are composed of either serous, mucous acini, or a combination of both. While the parotid gland is the largest of the three, all glands function to produce saliva to moisturize the mouth and assist in the breakdown of carbohydrates in the mouth. The submandibular gland is the primary source of basal saliva secretion, while the parotid gland is the main source of stimulated saliva secretion. The submandibular gland releases saliva through its main duct, Wharton’s duct, while the parotid gland and sublingual gland utilize Stensen’s duct and Bartholin’s duct respectively. Salivary glands also play a crucial immunologic role as their secretions contain many immunoglobins, namely IgA, that help fight bacteria and other foreign antigens in the oropharyngeal environment.<br />Histochemistry and Cytochemistry<br />Salivary glands are made up of three cell types: acinar cells, ductal cells, and myoepithelial cells. The myoepithelial cells are a crucial component of the glands as they wrap around both the ductal cells and acinar cells and contract to squeeze the saliva out of the gland. On hematoxylin and eosin (H & E) staining, the sublingual gland stains lighter than the parotid and submandibular glands. This staining is due to the heavy presence of glycolipids found in the sublingual gland secretions that give it a clear cytoplasmic appearance histologically. The ducts are lined with simple columnar epithelium and surrounded by a basal layer of myoepithelial cells. Enzymes (such as salivary peroxidase and salivary amylase) and peptides (including defensins, agglutinins, and cystatins) are stored in granules within the acinar cells, awaiting the signal for release as a component of the saliva. These granules stain darkly with hematoxylin, gray with mucicarmine, black with anti-smooth muscle actin (SMA), and rich brown with anti-amylase. Damage to the salivary glands is often evidenced histologically as the columnar cells become almost cuboidal, and the adipose tissue and surrounding stroma occupy more space as the cells balloon outwards .<br />