Peripheral Polyneuropathy
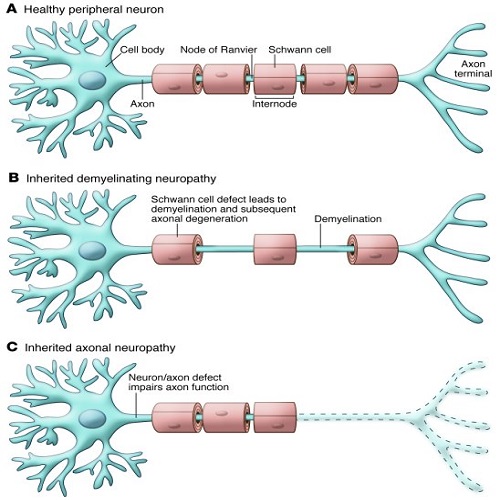
Peripheral Neuron:<br />It refers to the nerves outside brain &spinal cord. That divided into<br /> Sensory fiber <br /> Motor fiber<br /> Autonomic nerve fibers.<br /><br />Peripheral Polyneuropathy<br /> Polyneuropathy is the simultaneous malfunction of many peripheral nerves throughout the body . <br />Polyneuropathy may be presented as:<br /> Acute (beginning suddenly)<br /> Chronic (developing gradually, often over months or year)<br /> Most patients with polyneuropathy first present with a combination of sensory and motor symptoms and signs in the feet and lower legs, which later spread proximally in the legs and then into the hands and arms. Sometimes it can involve other parts of the body such as the autonomic nervous system.<br /> Peripheral polyneuropathy can be classified clinically according to the pathophysiology into:<br />• Axonal <br />• Demyelinating. <br />This classification is often helpful in identification of potential causes. <br /> <br />Figure(1.1) show the pathophysiology of peripheral polyneuropathy(Axonal & demyelinating )<br />Causes of Polyneuropathy:<br />1. Acute polyneuropathies <br />• Autoimmune reaction (when the body attacks its own tissues), as occurs in Guillain-Barré syndrome<br />• Alcohol & Toxins ( including side effects of medication)<br />2. Chronic Polyneuropathies:<br />• Diabetes (the most common)<br />• Excessive use of alcohol.<br />• Infections (such as hepatitis C, HIV infection) <br />• Hereditary neuropathies (such as Charcot-Marie-Tooth disease)<br />• Autoimmune disorders (e.g chronic inflammatory demyelinating polyneuropathy<br />• Vitamin B12 deficiency ,Kidney failure &Cancer<br /><br /> There are too many different types of polyneuropathy to be discussed. So we will discuss the most common types of acquired polyneuropathies such as acute inflammatory demyelinating polyneuropathy (Guillain–Barré syndrome), for acute type and diabetic neuropathy, B12 deficiency polyneuropathy (for chronic type of polyneuropathy).<br /> Guillain–Barre syndrome (GBS) : is an inflammatory polyneuropathy characterized by a progressive flaccid ascending and symmetric muscle weakness associated with motor features and with or without sensory symptoms. Guillian Barre are the first to define this condition as a progressive motor deficit including more than one limb, often symmetric,<br />associated with hyporeflexia or areflexia and with the maximum deficit being attained within four weeks of onset. The diagnosis is based on the clinical presentation and neurological findings supported by CSF and electrophysiological features(Shastri etal.,2023).<br /> The features of autonomic dysfunction such as arrhythmias, postural hypotension and bladder disturbances are also associated with GBS, and their effective management helps in determining the prognosis . Moreover, up to a third of patients usually require mechanical ventilation due to significant bulbar and respiratory muscle weakness. Approximately 20–50% of patients are left with residual and significant disability. The rate of mortality differs among centers of care but ranges between 5 and 10%. <br /> The pathophysiology of GBS is the result of autoimmune processes, whereby both cell-mediated and humoral responses come into play. The immunobiology involves T- and B-cell responses, complement system , antiganglioside antibodies and molecular mimicry . Molecular mimicry deals with antecedent infection with microorganisms wherein identical epitopes are shared incidentally between microbial structures and nerve structures, leading to a cellular immune response. Microbes that have been significantly associated with GBS are Campylobacter jejuni, Mycoplasma pneumonia, Haemophilus influenza, Epstein–Barr virus, cytomegalovirus (CMV), varicella zoster virus and influenza virus, out of which the most frequently associated organism is C. jejuni.<br />The diagnosis of GBS is based on extensive clinical history and neurological examination, and supported by the results of electrophysiological studies and CSF findings. It is also important to rule out other differential diagnosis such as malignancy, stroke, vitamin deficiencies.<br /> The treatment of GBS may constitute plasma-pheresis that usually includes at least five exchanges over a period of one week. Alternatively, the<br />patient may be treated with intravenous immunoglobulin (IVIG).<br /><br /> DIABETIC NEUROPATHY<br />Diabetic neuropathy (DN) is caused by damage of nerves due to diabetes mellitus (DM). The most common form of DN include painful polyneuropathy, <br />autonomic neuropathy, and so on. DN occurs in the peripheral nerves for example, sensory nerves, motor nerves, and the autonomic nervous system. Because it could damage all organs and systems, several distinct signs and symptoms can be caused depending on the injured nervous system. <br /> Signs and symptoms by DN often develop gradually with the passing years. The common symptoms are as follows: numbness and/or tingling of extremities; burning or electric pain; dysesthesia; trouble with balance; dizziness; vision changes; and so on.<br />When it comes to the pathogenesis of DN, diverse factors are suggested to be involved. The most prominent change occurred in the small vessels by DM is narrowing in them. With disease progression, blood vessel abnormalities are seen aggravated with capillary basement membrane thickening and endothelial hyperplasia. All these abnormalities can cause diminished oxygen tension and hypoxia, which are the main factors provoking neuronal ischemia. Thus, small blood vessel dysfunction is thought to occur early in diabetes and parallel the progression of neural dysfunction. <br /> Electrophysiological studies including nerve conduction tests can be helpful for the diagnosis as well. They might show reduced functions in the peripheral nerves.<br /> For the treatment of DN, tight glucose control should be preceded . Next, numerous treatments can be applied to reduce pain and other symptoms includes: antiepileptic drugs (AEDs), tricyclic antidepressants (TCAs), serotonin-norepinephrine reuptake inhibitors (SNRIs), and capsaicin cream can be prescribed for the control of pain in the patients with DN.<br /><br /><br /> Vitamin B12 Deficiency Neuropathy <br /> Peripheral neuropathy can be caused by malnutrition as described above and a lack of vitamin B12, an essential dietary nutrient, is clearly associated with peripheral neuropathy. Vitamin B12 deficiency (B12D) can cause a lot of serious conditions such as vitamin B12 deficiency neuropathy (B12DN) and is known to be relatively common in elderly people.<br />Several causes are associated with vitamin B12 deficiency and they include a strict vegetarian diet , the dysfunction of stomach acids, malabsorption syndromes, pernicious anemia, unexplained anemia, pancreatic diseases, gastritis, gastric or small intestine surgeries, ileal resection, Crohn’s disease, HIV infection, multiple sclerosis, use of proton pump inhibitors and so on.<br /> B12D can cause nerve damage, spinal cord degeneration as well as serious anemia. B12D induces the damage of the myelin sheath surrounding and protecting nerves. The damage of the myelin sheath makes nerves not function properly and leads to B12DN. If the underlying disease provoking B12D is not cured, the damage of the nerves induced by B12D might be permanently debilitating. Diverse symptoms can happen in B12DN: for example, numbness, tingling, and pain in feet and/or hands; sensory loss; lack of coordination; weakness; and so forth.<br />References: <br />1. Shastri, A , Al Aiyan, A , Kishore, U and Farrugia, M(2023).Immune-Mediated Neuropathies: Pathophysiology and Management., International Journal of molecular science, 24, 7288:(1-29).<br />2. Castelli, G., Desa,K., Canton,R.,(2020). Peripheral Neuropathy: Evaluation and Differential Diagnosis., American Family Physician 102 (12):732 -739.<br /><br /> اعداد<br /> د.زهراء طارق حسون