Neuro Monitoring During General Anesthesia in Surgery
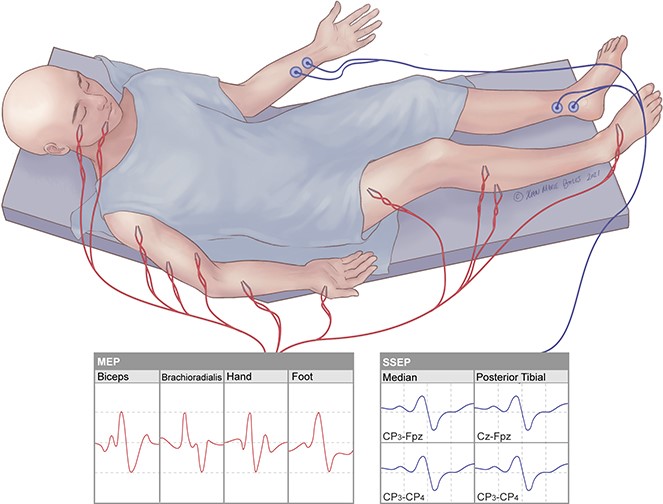
Neuro monitoring during general anesthesia is a critical component in modern anesthetic practice. Its purpose is to ensure that the central nervous system (CNS) is protected during surgery, particularly in cases where there is a risk of neurological injury due to the nature of the surgery or the anesthetic techniques used. This lecture will provide an overview of the types of neuro monitoring used in surgery, the principles behind them, and their applications in general anesthesia.<br />1. What is Neuro Monitoring in Anesthesia?<br />Neuro monitoring refers to the continuous or intermittent assessment of neural function during a surgical procedure. The goal is to detect changes in neural activity or integrity as early as possible, allowing for prompt intervention to prevent neurological damage.<br />During general anesthesia, there are several factors that could potentially affect the nervous system, including:<br />• Direct injury (e.g., from surgical instruments)<br />• Ischemia (reduced blood flow to the brain or spinal cord)<br />• Hypoxia (low oxygen levels)<br />• Pressure on nerves or brain tissue (e.g., positioning)<br />• Metabolic changes (e.g., electrolyte imbalances)<br />Neuro monitoring techniques help anesthesiologists, surgeons, and neurophysiologists detect early signs of distress or dysfunction in the CNS.<br />2. Types of Neuro Monitoring Techniques<br />There are several different types of neuro monitoring that are commonly used during general anesthesia in surgery. These can be broadly categorized into two groups: electrophysiological monitoring and imaging techniques. However, electrophysiological monitoring is the most common in real-time surgical environments.<br />a. Electroencephalogram (EEG) Monitoring<br />• Purpose: EEG monitoring is used to assess the brain's electrical activity during surgery. It is often employed to monitor the depth of anesthesia.<br />• How it works: Electrodes are placed on the scalp to record brainwave patterns. An anesthesiologist can adjust anesthetic drugs based on EEG readings to maintain an appropriate level of anesthesia, reducing the risk of awareness during surgery and minimizing the chances of overdose.<br />• Applications: Especially useful in long surgeries, particularly those involving the brain (e.g., neurosurgeries), and for monitoring for potential seizures.<br />b. Somatosensory Evoked Potentials (SSEP)<br />• Purpose: SSEPs are used to monitor the sensory pathways from the peripheral nervous system to the brain, providing valuable information about spinal cord function.<br />• How it works: Electrical stimuli are applied to a peripheral nerve, and the response is measured at the cortex, indicating the integrity of sensory pathways. Any delay or loss of response may indicate nerve compression, ischemia, or other issues.<br />• Applications: Commonly used in spinal surgeries, particularly those that involve the cervical spine or spinal cord.<br />c. Motor Evoked Potentials (MEP)<br />• Purpose: MEPs assess motor pathways, particularly the corticospinal tract, to monitor for potential damage during surgery.<br />• How it works: A small electrical stimulus is applied to the brain or spinal cord, and the muscle response is measured. A decrease in motor response can indicate issues with the motor pathways or spinal cord injury.<br />• Applications: Used in spinal surgeries, particularly in the cervical or thoracic spine, and during surgeries involving the brain or brainstem.<br />d. Transcranial Doppler Ultrasonography (TCD)<br />• Purpose: TCD monitors cerebral blood flow and provides real-time information on cerebral circulation.<br />• How it works: A probe is placed over the skull to measure the velocity of blood flow through major brain arteries. Abnormalities in blood flow can indicate compromised cerebral perfusion, potentially leading to ischemia or stroke.<br />• Applications: Used in surgeries where cerebral perfusion may be at risk, such as in major cardiovascular surgeries or neurosurgical procedures.<br />e. Bispectral Index (BIS) Monitoring<br />• Purpose: BIS is a method of monitoring the depth of anesthesia to ensure the patient remains unconscious during surgery.<br />• How it works: The BIS system analyzes EEG signals to produce a numerical score (0-100). A lower score indicates deeper anesthesia, and a higher score suggests a lighter plane of anesthesia.<br />• Applications: Common in routine surgeries to monitor anesthetic depth and prevent intraoperative awareness.<br />3. Importance of Neuro Monitoring in Surgery<br />The role of neuro monitoring in surgical settings cannot be overstated. It serves several key functions:<br />a. Protecting Neural Integrity<br />• Many surgical procedures, especially those involving the spine or brain, carry a risk of accidental nerve or spinal cord damage. Neuro monitoring enables real-time detection of any abnormal neural activity or electrical signals, allowing for prompt action to prevent long-term damage.<br />b. Ensuring Adequate Anesthesia Depth<br />• Monitoring tools such as EEG and BIS allow anesthesiologists to titrate anesthetic agents effectively, preventing both under- and over-anesthesia. Under anesthesia, the patient may experience awareness, while excessive anesthesia may lead to side effects such as hypotension and organ dysfunction.<br />c. Guiding Surgical Decisions<br />• For certain procedures, the surgeon may rely on neurophysiological feedback to guide their actions. For example, in spinal surgery, SSEPs and MEPs provide feedback on whether any manipulation of the spine is compromising neural function, allowing the surgeon to adjust their approach.<br />d. Early Detection of Complications<br />• Abnormal changes in neural activity detected during monitoring can provide early warning signs of complications such as ischemia, hypoxia, or surgical trauma. This allows for earlier intervention to avoid permanent damage.<br />4. Challenges and Limitations of Neuro Monitoring<br />While neuro monitoring is a powerful tool, it does come with its own set of challenges and limitations:<br />a. Interpretation of Results<br />• The interpretation of neuro monitoring data requires expertise, and in some cases, results may be ambiguous or difficult to interpret. It is crucial to have skilled neurophysiologists or anesthesiologists interpreting the data in real-time.<br />b. Anesthesia Interference<br />• Certain anesthetic agents (e.g., volatile anesthetics or muscle relaxants) can interfere with neuro monitoring readings. For example, the use of muscle relaxants can distort MEP results. Anesthesiologists must adjust the monitoring techniques to account for these effects.<br />c. Technical Challenges<br />• Proper electrode placement is critical for accurate readings, and technical issues such as poor electrode contact, electrical interference, or patient movement can compromise the quality of the data.<br />d. Cost and Equipment<br />• Neuro monitoring equipment can be expensive, and not all hospitals or surgical centers have access to the necessary technology or expertise. Additionally, continuous monitoring can be labor-intensive, requiring additional personnel and resources.<br />5. Clinical Applications of Neuro Monitoring<br />Neuro monitoring is especially valuable in surgeries where the nervous system is at particular risk. Some common clinical applications include:<br />a. Spinal Surgery<br />• SSEPs and MEPs are commonly used to monitor the integrity of the spinal cord during procedures such as laminectomies, spinal fusions, or scoliosis correction. Early changes in these readings can alert the surgical team to potential spinal cord injury.<br />b. Neurosurgery<br />• During brain surgery (e.g., tumor resection, epilepsy surgery, or vascular surgery), EEG monitoring helps detect abnormal brain activity, and TCD can monitor cerebral blood flow. This ensures that the brain remains adequately perfused and protected.<br />c. Carotid Endarterectomy<br />• TCD is frequently used during carotid endarterectomy to monitor cerebral perfusion and detect signs of cerebral ischemia during the surgery, which can help prevent stroke.<br />d. Cardiac Surgery<br />• In complex cardiac surgeries, such as open-heart surgery, neuro monitoring is used to ensure that blood flow to the brain is maintained and that there is no risk of stroke or other neurological complications.<br />6. Conclusion<br />Neuro monitoring during general anesthesia is a vital aspect of ensuring patient safety in surgeries that pose a risk to the nervous system. The ability to detect early signs of neurological dysfunction allows for timely interventions that can significantly reduce the risk of permanent damage. As technology advances, the integration of these monitoring techniques will continue to improve patient outcomes, particularly in high-risk surgeries.<br />For anesthesiologists, surgeons, and other medical professionals, the ability to effectively utilize neuro monitoring is crucial for both the immediate management of the patient during surgery and long-term post-operative care. Continuing education and collaboration between anesthesia providers and neurophysiologists will be key to maximizing the benefits of these technologies in the future.<br /><br />د. محمد سامي <br /><br /><br /><br /><br />The first university in Iraq