Awake Brain Surgery: Techniques, Benefits, and Considerations
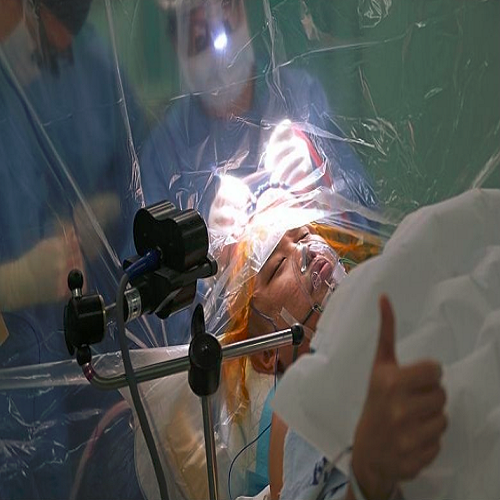
Introduction<br />Awake brain surgery, also known as awake craniotomy or awake neurosurgery, is a specialized technique used in certain types of brain surgeries where the patient remains conscious during the procedure. This approach allows surgeons to map out critical areas of the brain, avoid damage to essential functions (such as speech, movement, or sensation), and reduce the risk of postoperative complications.<br />While the idea of being awake during brain surgery might seem unsettling, it is often the best option for specific conditions, particularly when the tumor or lesion is near functional brain areas. In this lecture, we will explore the principles behind awake brain surgery, its indications, the techniques used, and the unique benefits and challenges it presents.<br />1. What is Awake Brain Surgery?<br />Awake brain surgery involves performing surgery on a patient while they are awake, with local anesthesia used to numb the scalp and surrounding tissues. However, the patient remains conscious and able to respond to commands or questions during parts of the procedure, particularly when the surgeon needs to test or map brain function.<br />Unlike traditional brain surgery, where the patient is fully anesthetized, awake surgery enables real-time feedback from the patient to ensure that critical brain functions—such as language, movement, and sensation—are preserved during the procedure.<br />2. Indications for Awake Brain Surgery<br />Awake brain surgery is often considered in cases where the brain lesion (tumor, vascular malformation, or epileptic focus) is located near or within areas of the brain responsible for crucial functions, such as:<br />• Language centers: For tumors or lesions near Broca’s area or Wernicke’s area, which control speech and comprehension.<br />• Motor function areas: For lesions affecting the motor cortex, where movement control is coordinated.<br />• Sensory areas: When tumors or lesions are located near sensory regions that control touch, vision, or other sensations.<br />• Epilepsy surgery: For patients with epilepsy, awake surgery can help locate the focus of seizures so it can be removed or treated.<br />The primary goal of awake surgery is to remove as much of the tumor or lesion as possible while preserving the brain’s functional areas. This is critical in minimizing the chances of neurological deficits after the surgery.<br />3. The Process of Awake Brain Surgery<br />a. Preoperative Preparation<br />Before the surgery, the patient undergoes several evaluations to determine their suitability for the procedure:<br />• Imaging studies: High-resolution MRI, functional MRI (fMRI), and sometimes positron emission tomography (PET) are used to map the location of the tumor in relation to critical brain areas. fMRI helps identify regions involved in language, motor control, and sensory function.<br />• Cognitive testing: Preoperative cognitive tests assess the patient’s baseline abilities in language, memory, and motor skills. This establishes a baseline for comparison during surgery.<br />b. Anesthesia and Sedation<br />During awake brain surgery, the patient is typically given a combination of local anesthesia and sedation. The key steps include:<br />• Scalp anesthesia: Local anesthetics are injected into the scalp to numb the area of the head where the incision will be made.<br />• Sedation: A mild sedative (e.g., an IV infusion of propofol) is given to keep the patient calm and comfortable without making them fully unconscious. The goal is to ensure the patient remains relaxed but aware enough to follow instructions.<br />c. Intraoperative Mapping and Monitoring<br />Once the patient is sedated and their scalp is anesthetized, the procedure begins. The surgery itself proceeds in several key stages:<br />• Craniotomy: The surgeon makes an incision in the scalp and removes a small section of the skull to access the brain.<br />• Cortical mapping: The surgeon may use electrical stimulation to map the brain’s motor, sensory, and language areas. During this step, the patient is asked to perform tasks (such as speaking, moving a limb, or feeling stimuli) to assess the brain’s function.<br />o Example: The patient may be asked to say words or count numbers while the surgeon stimulates different areas of the brain. If the stimulation causes a temporary speech or motor disruption, the surgeon knows that area is critical for that function and must be preserved.<br />• Awake monitoring: Throughout the surgery, the patient’s responses are carefully monitored. The anesthesiologist and surgical team ensure the patient is comfortable and able to communicate.<br />d. Tumor or Lesion Removal<br />With real-time feedback from the patient, the surgeon proceeds with the removal of the tumor or lesion. The key advantage of awake surgery is the ability to remove tissue near critical functional areas while minimizing damage to them. In some cases, the patient may be asked to perform tasks (such as counting or moving fingers) during the surgery to ensure that critical functions are preserved.<br />Once the lesion is removed, the surgical site is closed, and the patient is carefully monitored in the recovery room.<br />4. Benefits of Awake Brain Surgery<br />The primary advantage of awake brain surgery is its ability to preserve neurological function while removing brain tumors or lesions. Some of the specific benefits include:<br />a. Real-time Functional Mapping<br />• Preservation of critical functions: By directly stimulating and testing different regions of the brain, the surgeon can map out areas that control vital functions such as speech, movement, and sensation, ensuring they are preserved during surgery.<br />• Maximal tumor removal: The surgeon can safely remove more of the tumor or lesion, especially if it is located near these functional areas, without compromising the patient’s ability to perform basic tasks like speaking or moving.<br />b. Reduction of Postoperative Deficits<br />• Fewer neurological deficits: Awake surgery helps avoid damaging important brain structures, reducing the likelihood of postoperative deficits (e.g., speech difficulties, motor impairments, sensory loss).<br />• Improved recovery: Because critical brain functions are preserved, recovery is often quicker and more complete compared to traditional brain surgery.<br />c. Informed Decision-Making<br />• Patient involvement: Awake surgery allows patients to be involved in their care. For example, if a patient experiences temporary motor or speech deficits during the procedure, the surgeon can make real-time decisions about how to proceed with the surgery.<br />5. Challenges and Considerations<br />Despite its benefits, awake brain surgery comes with challenges and requires careful consideration:<br />a. Psychological Impact<br />• Anxiety and discomfort: Some patients may experience anxiety or discomfort about being awake during surgery. Preoperative counseling and psychological support are critical for patient comfort.<br />• Unpredictable reactions: Not all patients respond the same way to sedation or anesthesia, and some may become too anxious or uncomfortable during the procedure.<br />b. Complexity and Time<br />• Longer surgical time: Awake surgery may take longer than traditional surgery because of the need for careful mapping and patient interaction.<br />• Highly specialized team: It requires an experienced neurosurgical team, including anesthesiologists, neurophysiologists, and neuropsychologists, to ensure the patient’s safety and comfort.<br />c. Risks and Safety<br />• Seizure risk: During the surgery, brain stimulation can potentially trigger seizures, especially in patients with epilepsy or brain lesions prone to electrical activity.<br />• Patient discomfort: Despite sedation, the patient may experience discomfort during certain parts of the procedure, particularly if the brain is being stimulated or if the head is held in a fixed position for long periods.<br />6. Clinical Applications<br />Awake brain surgery is particularly useful in certain types of brain surgery:<br />a. Tumor Resection<br />• Tumors that are located near critical brain functions (e.g., in the frontal lobe or temporal lobe) benefit from awake surgery because the surgeon can ensure they don’t damage speech, motor, or sensory regions.<br />b. Epilepsy Surgery<br />• For patients with drug-resistant epilepsy, awake surgery can be used to locate and remove the focus of seizures, improving the patient's quality of life.<br />c. Functional Neurosurgery<br />• In surgeries where functional outcomes are critical—such as those involving the motor cortex, speech areas, or sensory regions—awake surgery is invaluable for protecting these functions during resection.<br /><br /><br />د. محمد سامي <br /><br /><br /><br /><br />The first university in Iraq