Fibrous Dysplasia and Pregnancy
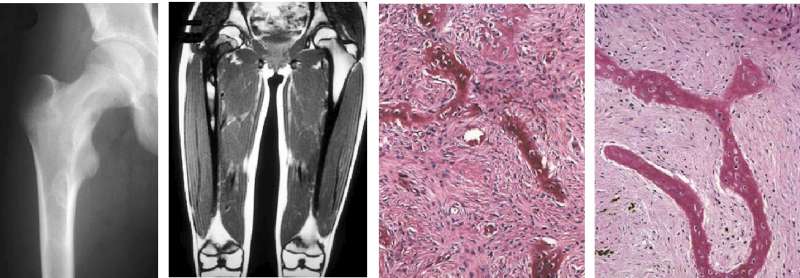
Fibrous dysplasia (FD) is a rare skeletal disorder characterized by the replacement of normal bone with fibrous connective tissue, leading to structural weakness, deformities, and potential fractures. The condition arises from a mutation in the GNAS gene, resulting in the overproduction of cyclic adenosine monophosphate (cAMP) and subsequent disruption of normal bone development. FD can occur in monostotic (single bone) or polyostotic (multiple bones) forms and may be associated with endocrine abnormalities, such as in McCune-Albright Syndrome (MAS). Pregnancy presents unique challenges for individuals with FD, as hormonal changes and mechanical stresses can exacerbate symptoms and complicate management.<br />Impact of Pregnancy on Fibrous Dysplasia<br />1. Hormonal Influences Pregnancy induces significant hormonal changes, including elevated levels of estrogen, progesterone, and relaxin. These hormones can influence the metabolic activity of bone, potentially exacerbating FD lesions. Estrogen, for example, is known to modulate bone turnover, which might increase the risk of pain or fractures in affected areas. Relaxin, which promotes ligamentous relaxation and joint mobility, may further compromise the structural integrity of bones weakened by FD.<br />2. Mechanical Stress The additional weight gain and altered biomechanics of pregnancy can place increased stress on bones affected by FD. This is particularly concerning in polyostotic cases or when weight-bearing bones such as the femur or pelvis are involved. Patients may experience worsening of bone pain or deformities, and fractures may occur more easily under the additional strain.<br />3. Potential for Endocrine Activation In cases of FD associated with MAS, pregnancy-related hormonal changes might activate or exacerbate endocrine abnormalities. For instance, preexisting hyperthyroidism or growth hormone excess can worsen during pregnancy, requiring careful monitoring and management to avoid complications for both the mother and fetus.<br />Clinical Management During Pregnancy<br />Managing FD during pregnancy requires a multidisciplinary approach, involving obstetricians, endocrinologists, orthopedic specialists, and, in some cases, pain management experts. Key considerations include:<br />1. Preconception Counseling Women with FD should undergo thorough preconception counseling to assess the extent of their disease, particularly focusing on skeletal deformities, endocrine function, and prior complications. Imaging studies and laboratory tests may be performed to determine the potential risks associated with pregnancy.<br />2. Monitoring During Pregnancy Regular monitoring is essential to address potential complications promptly. This may include:<br />o Bone health: Periodic assessment of pain, mobility, and signs of fractures or deformities.<br />o Endocrine function: Monitoring for changes in thyroid, adrenal, or growth hormone activity, particularly in MAS.<br />o Fetal health: Ensuring that maternal complications do not adversely affect fetal development.<br />3. Pain Management Pain is a common symptom of FD and may worsen during pregnancy. Nonpharmacological interventions, such as physical therapy and supportive devices, should be prioritized. When medications are necessary, acetaminophen is generally considered safe. Nonsteroidal anti-inflammatory drugs (NSAIDs) should be used with caution, especially in the third trimester due to potential adverse effects on the fetus.<br />4. Fracture Prevention and Management Preventing fractures is a critical aspect of care. Patients may benefit from assistive devices, such as crutches or braces, to reduce stress on affected bones. If a fracture occurs, conservative management with immobilization is preferred unless surgical intervention is unavoidable. Surgical options may be limited during pregnancy due to the risks associated with anesthesia and radiation exposure from imaging.<br /><br />Obstetric Considerations<br />1. Mode of Delivery The mode of delivery should be carefully planned based on the patient’s skeletal involvement. For instance:<br />o Vaginal delivery may be feasible in cases of mild FD without significant pelvic involvement.<br />o Cesarean delivery may be recommended for patients with severe pelvic deformities or fractures to minimize the risk of complications.<br />2. Anesthesia Anesthesia planning should account for potential skeletal abnormalities, particularly in the spine. Epidural or spinal anesthesia may be challenging in patients with FD-related spinal deformities, necessitating consultation with an anesthesiologist.<br />3. Postpartum Care Postpartum recovery may be prolonged in women with FD, especially if fractures or significant pain occurred during pregnancy. Lactation-associated hormonal changes may also temporarily influence bone health, requiring additional monitoring.<br />Research and Future Directions<br />Limited research exists on the interaction between FD and pregnancy, underscoring the need for further studies to establish evidence-based guidelines. Areas of interest include:<br />• The impact of pregnancy-related hormones on FD progression.<br />• Optimal pain management strategies during pregnancy.<br />• Long-term outcomes for mothers and offspring.<br />Conclusion<br />Pregnancy in women with fibrous dysplasia presents unique challenges requiring careful planning and multidisciplinary management. Hormonal changes, mechanical stress, and potential endocrine complications necessitate vigilant monitoring to ensure favorable maternal and fetal outcomes. With appropriate care, many women with FD can experience successful pregnancies and childbirth, though individualized treatment plans are essential to address their specific needs.<br /><br /><br />Future University is the first university in Iraq