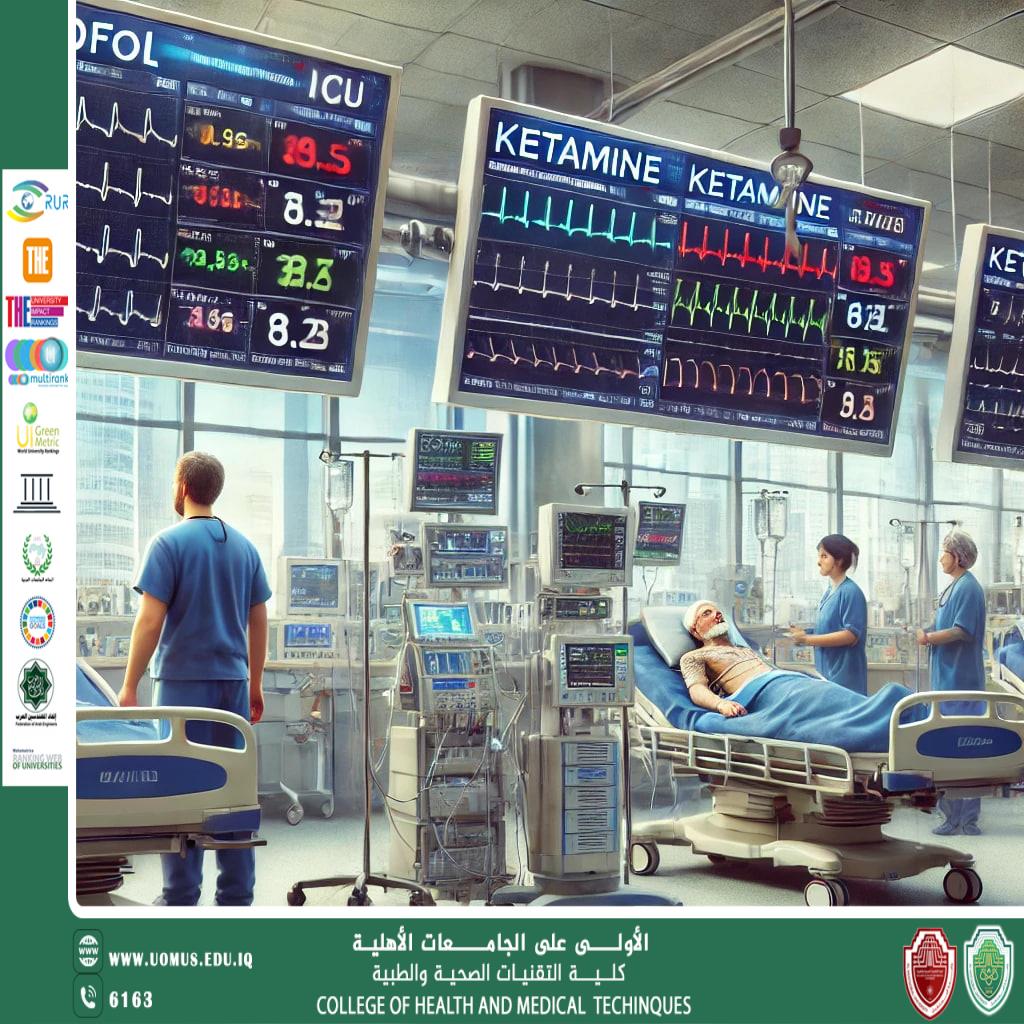
Comparative Study of Propofol and Ketamine on Hemodynamic Parameters in Intensive Care Unit Patients
Optimal sedation in the Intensive Care Unit (ICU) is essential for effective patient <br />management, particularly in critically ill patients requiring mechanical ventilation and <br />procedural sedation. However, sedation-related hemodynamic instability remains a <br />significant concern. This expanded review explores the comparative effects of propofol and<br />ketamine on hemodynamic parameters, including blood pressure, heart rate, and <br />cardiovascular stability, offering advanced insights for clinical practice. We analyze the <br />mechanisms of action, recent clinical trials, and practical implications for sedative choice in<br />ICU patients.<br />Introduction<br />Significance of Hemodynamic Stability in ICU Patients<br />Patients in the ICU often require sedation for mechanical ventilation, invasive procedures, <br />and pain management. However, the sedative agents used must balance efficacy and <br />safety while minimizing adverse hemodynamic effects, which can impact perfusion, <br />oxygenation, and organ function.<br />Why Compare Propofol and Ketamine?<br />Propofol and ketamine are two widely used intravenous sedatives in critical care, but they <br />have opposing hemodynamic profiles:<br />. Propofol: Induces dose-dependent hypotension and bradycardia due to vasodilation and <br />myocardial depression.<br />. Ketamine: Acts as a cardiovascular stimulant, increasing heart rate and blood pressure, <br />making it potentially useful in hemodynamically unstable patients.<br />This article provides an in-depth comparison of their effects on cardiovascular parameters <br />to guide clinicians in optimizing sedation protocols for ICU patients.<br />Pharmacological Profiles of Propofol and Ketamine<br />1. Propofol<br />Mechanism of Action<br />. Acts on GABA-A receptors, enhancing inhibitory neurotransmission.<br />. Rapid onset (30-60 seconds) and short duration (3-10 minutes).<br />. Highly lipophilic, leading to fast redistribution.<br />Hemodynamic Effects<br />. Peripheral vasodilation reduces systemic vascular resistance (SVR).<br />. Myocardial depression lowers cardiac output and blood pressure.<br />. Dose-dependent bradycardia due to vagal stimulation.<br />2. Ketamine<br />Mechanism of Action<br />. NMDA receptor antagonist, leading to dissociative anesthesia.<br />. Enhances sympathetic outflow, increasing catecholamine release.<br />. Provides analgesia, amnesia, and bronchodilation.<br />Hemodynamic Effects<br />. Increases heart rate and blood pressure via sympathetic activation.<br />. Maintains cardiac output, making it suitable for hypotensive patients.<br />. Minimal respiratory depression, unlike propofol.<br />Comparative Hemodynamic Effects<br />1. Effects on Blood Pressure<br />Propofol<br />. Significant hypotension observed, particularly in elderly and hypovolemic patients.<br />. Can cause profound blood pressure drops in septic and trauma patients due to <br />vasodilation and negative inotropy.<br />Ketamine<br />. Increases mean arterial pressure (MAP) due to sympathetic stimulation.<br />. Maintains peripheral vasoconstriction, useful in shock states.<br />Clinical Evidence:<br />. A study by Atchley et al. (2022) found that ketamine caused significantly less hypotension<br />compared to propofol or dexmedetomidine (34.6% vs. 63.5%; P < 0.001) (PubMed).<br />. Egyptian Journal of Hospital Medicine (2024): Ketamine led to higher MAP values at <br />various time points compared to propofol, supporting its role in hemodynamically unstable <br />patients (EJHM).<br />2. Effects on Heart Rate<br />Propofol<br />. Dose-dependent bradycardia due to baroreceptor suppression.<br />. May require vasopressor support (e.g., norepinephrine) in hypotensive patients.<br />Ketamine<br />. Increases heart rate due to catecholamine release.<br />. Avoid in cardiac patients at risk of tachyarrhythmias.<br />Clinical Evidence:<br />. A study on pediatric patients undergoing cardiac catheterization found higher heart rates <br />with ketamine than with propofol (BriefLands).<br />3. Effects on Cardiac Output and Systemic Vascular Resistance<br />. Propofol reduces cardiac output and SVR, worsening hypotension in sepsis or <br />hypovolemia.<br />. Ketamine maintains or increases cardiac output, useful in hypovolemic or trauma <br />patients.<br />Clinical Implications of Sedative Choice<br />Ketamine<br />. Blood Pressure (Hypertension)<br />. Heart Rate (Tachycardia)<br />. Cardiac Output (Maintenance)<br />. Best For Hemodynamically unstable patients (e.g., shock, sepsis)<br />Propofol<br />. Blood Pressure (Hypotension)<br />. Heart Rate (Bradycardia)<br />. Cardiac Output (Depression) <br />. Best For Patients needing BP reduction (e.g., hypertension, cerebral aneurysms)<br />Propofol Use Cases<br />. Patients with intracranial hypertension (lowers cerebral perfusion pressure).<br />. Patients requiring tight BP control (e.g., post-cardiac surgery).<br />Ketamine Use Cases<br />. Septic shock, trauma, or hemorrhagic shock (maintains perfusion).<br />. Bronchospasm or asthma patients (bronchodilator effect).<br />Advanced Insights and Recent Developments<br />1. Propofol-Ketamine Combination (“Ketofol”)<br />. Rationale: Offsets propofol-induced hypotension while reducing ketamine-induced <br />tachycardia.<br />. Studies suggest this combination results in:<br />. More stable hemodynamics.<br />. Less respiratory depression.<br />. Better sedation quality.<br />Clinical Trial Reference:<br />• Ali et al. (2022): “Ketofol administration resulted in improved hemodynamic stability <br />compared to propofol alone during intubation and maintenance of anesthesia”<br />(ResearchGate).<br />2. Hemodynamic Effects on Cerebral Oxygenation<br />. Propofol may decrease cerebral perfusion, affecting neurological patients.<br />. Ketamine maintains cerebral blood flow, but may increase intracranial pressure.<br />Neurocritical Care Consideration:<br />. Propofol preferred for brain injury patients with high ICP.<br />. Ketamine beneficial in hypotensive brain injury patients.<br />Conclusion and Future Directions<br />Key Takeaways:<br />. Propofol is cardiodepressant, ideal for patients needing controlled hypotension.<br />. Ketamine is hemodynamically stable, useful for hypotensive patients.<br />. Combination (“Ketofolâ€) offers balanced sedation with reduced side effects.<br />Future Research Areas<br />. Large-scale randomized controlled trials on propofol-ketamine synergy.<br />. Long-term impact on neurological and cardiovascular outcomes.<br />. Personalized sedation protocols based on genetic and metabolic factors.<br />References<br />1. Atchley, E. et al. (2022). Hemodynamic Effects of Ketamine Compared with Propofol or <br />Dexmedetomidine as Continuous ICU Sedation. Annals of Pharmacotherapy. (PubMed)<br />2. Ali, Z. et al. (2022). The Effect of Ketamine-Propofol Administration on Hemodynamic <br />Stability. ResearchGate. (ResearchGate)<br />3. Egyptian Journal of Hospital Medicine (2024). (EJHM<br />م.محمد خضير عباس<br /><br />Al-Mustaqbal University is the first university in Iraq