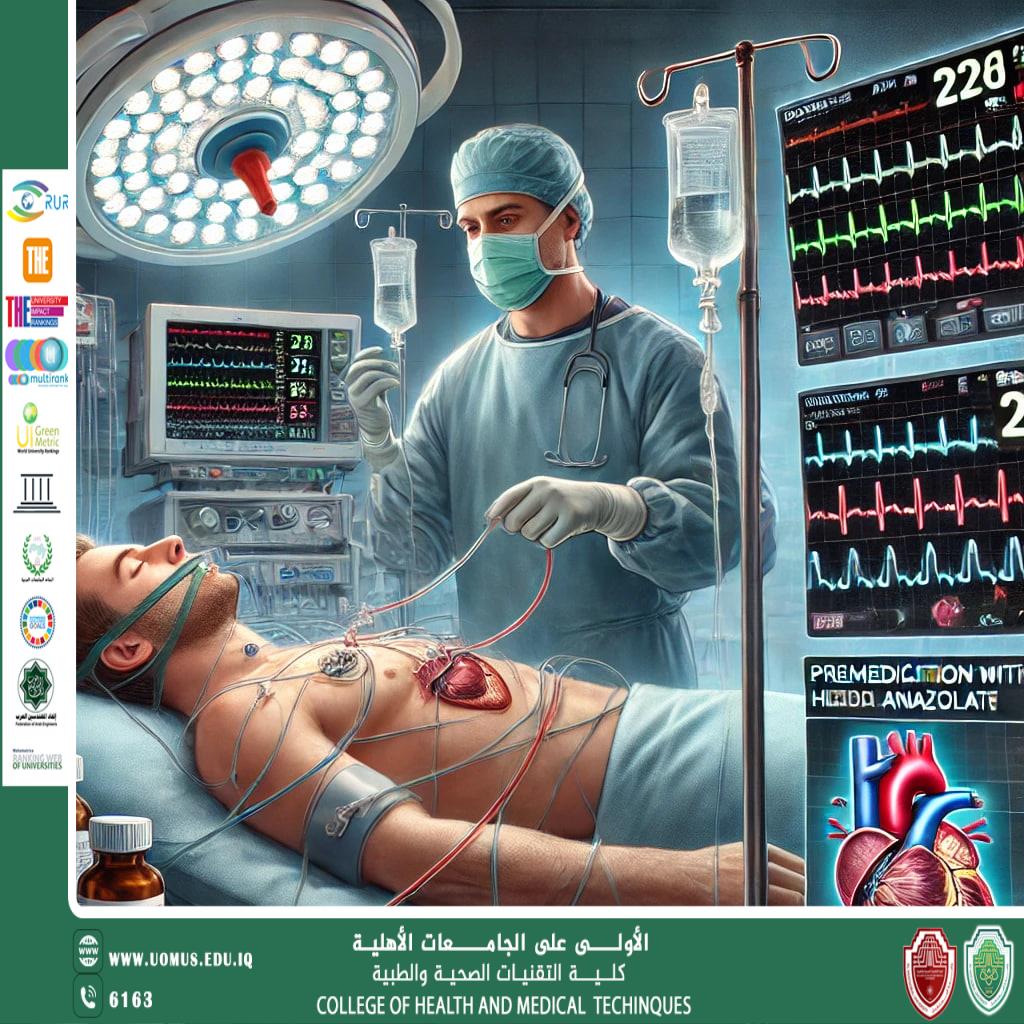
The Effect of Premedication with Midazolam on Heart Rate During General Anesthesia
Midazolam, a widely used benzodiazepine, is a key premedication agent in anesthesia due<br />to its anxiolytic, amnestic, muscle relaxant, and sedative properties. Its impact on <br />hemodynamic parameters, particularly heart rate (HR), has been extensively studied to <br />optimize anesthesia protocols. While midazolam generally exerts a cardiostabilizing effect,<br />its influence on HR can vary depending on dosage, patient condition, and concurrent <br />anesthetic agents.<br />This review explores the mechanism of action of midazolam, its effect on HR regulation <br />during general anesthesia, comparative studies with other premedication agents, and its <br />clinical implications in various surgical populations.<br />Introduction<br />Rationale for Premedication in General Anesthesia<br />Premedication is administered before induction of anesthesia to:<br />. Reduce anxiety and psychological stress before surgery.<br />. Minimize autonomic instability, including fluctuations in HR and blood pressure (BP).<br />. Facilitate smooth anesthetic induction and decrease anesthetic drug requirements.<br />. Improve patient comfort in the perioperative setting.<br />Midazolam is a first-line benzodiazepine for premedication due to its rapid onset, short <br />half-life, and high safety profile. However, its effect on HR remains an area of clinical <br />interest because HR changes can impact cardiac output, oxygen delivery, and <br />perioperative complications.<br />Mechanism of Action of Midazolam and Its Cardiovascular Effects<br />1. GABA-A Receptor Modulation<br />. Midazolam acts by enhancing gamma-aminobutyric acid (GABA) transmission, leading to<br />CNS depression.<br />. This results in sedation, anxiolysis, and mild muscle relaxation without significant <br />respiratory depression at premedication doses.<br />2. Autonomic Nervous System Modulation<br />. Midazolam inhibits excessive sympathetic nervous system (SNS) activation, leading to a <br />reduction in stress-induced tachycardia.<br />. It has a dose-dependent effect on HR, with higher doses causing a slight decrease in HR <br />due to vagal stimulation.<br />3. Preservation of Hemodynamic Stability<br />. Unlike opioids or alpha-2 agonists (e.g., clonidine, dexmedetomidine), midazolam does <br />not cause profound bradycardia.<br />. It helps maintain a stable HR and BP, reducing hemodynamic fluctuations during <br />induction and intubation.<br />Effect of Midazolam on Heart Rate During General Anesthesia<br />1. HR Reduction Due to Sympatholytic Effect<br />Key Finding: Midazolam reduces stress-induced tachycardia by suppressing SNS <br />activation.<br />. A study comparing midazolam and diazepam premedication found that both agents <br />reduced HR upon arrival in the operating room, particularly in elderly patients.<br />. The reduction was attributed to attenuation of anxiety-induced sympathetic stimulation.<br />( Academic.oup.com )<br />2. No Significant HR Alteration at Low Doses<br />Key Finding: Low-dose midazolam (<0.05 mg/kg) does not significantly affect HR in <br />healthy adults.<br />. A randomized controlled trial assessing midazolam co-induction with general anesthesia <br />found that HR remained unchanged compared to control groups.<br />. Midazolam stabilized BP without causing excessive bradycardia or tachycardia.<br />( PMC.ncbi.nlm.nih.gov )<br />3. HR Increase Compared to Alpha-2 Agonists (e.g., Clonidine, Dexmedetomidine)<br />Key Finding: Midazolam premedication results in higher HR values compared to clonidine <br />or dexmedetomidine.<br />. A study comparing clonidine vs. midazolam premedication found that midazolam patients <br />had significantly higher HRs post-induction.<br />. This suggests that midazolam does not cause excessive vagal stimulation, unlike alpha-2<br />agonists.<br />( Journalajrs.com )<br />4. HR Variability (HRV) and Autonomic Balance<br />Key Finding: Midazolam premedication reduces HR variability (HRV), suggesting <br />autonomic modulation.<br />. A study on HRV changes following midazolam administration found that both low- and <br />high-frequency components of HRV were reduced.<br />. This indicates a decrease in autonomic nervous system activity, leading to a stable HR.<br />( Associationofanaesthetists-publications.onlinelibrary.wiley.com )<br />Comparative Studies: Midazolam vs. Other Premedication Agents<br />Premedication Agent,Effect on HR,Clinical Implications<br />Midazolam,Mild HR reduction or no change,Suitable for stable hemodynamics<br />Clonidine (alpha-2 agonist),Significant HR decrease (bradycardia),Preferred in <br />hypertensive patients<br />Dexmedetomidine (alpha-2 agonist),More pronounced HR reduction,Caution in <br />bradycardia-prone patients<br />Opioids (Fentanyl, Morphine),Variable HR effects (mild bradycardia possible),Risk of <br />hypotension and respiratory depression<br />Clinical Implications of Midazolam’s Effect on HR<br />1. Optimal Use in Patients with Anxiety-Induced Tachycardia<br />. Midazolam attenuates excessive HR elevation caused by preoperative stress.<br />. Useful in young, anxious patients or those with mild tachycardia.<br />2. Safer Alternative for Patients at Risk of Bradycardia<br />. Unlike clonidine or dexmedetomidine, midazolam does not cause profound bradycardia.<br />. Recommended for patients with baseline bradycardia or conduction abnormalities.<br />3. Need for Monitoring in Hemodynamically Unstable Patients<br />. In hypovolemic or elderly patients, midazolam may cause mild HR reduction, <br />necessitating BP and HR monitoring.<br />. Consider dose adjustments (0.025–0.05 mg/kg IV) in these populations.<br />Conclusion and Future Directions<br />Midazolam premedication modulates HR by reducing sympathetic activity, but its effects <br />are mild and dose-dependent. While it can attenuate stress-induced tachycardia, it does <br />not cause significant bradycardia, making it a hemodynamically safe choice for most <br />patients.<br />Future Research Areas<br />. Personalized dosing strategies based on patient age, autonomic function, and <br />comorbidities.<br />. Comparative trials evaluating midazolam vs. newer sedatives (e.g., remimazolam).<br />. Long-term HRV studies to assess midazolam’s effect on autonomic nervous system <br />recovery post-anesthesia.<br />References<br />1. Mihalj M, Karlović Z, et al. (2022). Effects of midazolam co-induction to general <br />anesthesia: A randomized clinical trial. Medicine, 101(45):e31400. (PMC)<br />2. Rahaman MA, Islam S, et al. (2023). Evaluating the comparative efficacy of midazolam <br />and clonidine as premedication agents. Asian J Res Surg. (JournalAJRS)<br />3. Michaloudis D, Kanakoudis F, et al. (1998). Influence of premedication on HRV. <br />Anaesthesia, 53(5):446-453. (Wiley<br /><br />م.محمد خضير عباس<br /><br />Al-Mustaqbal University is the first university in Iraq