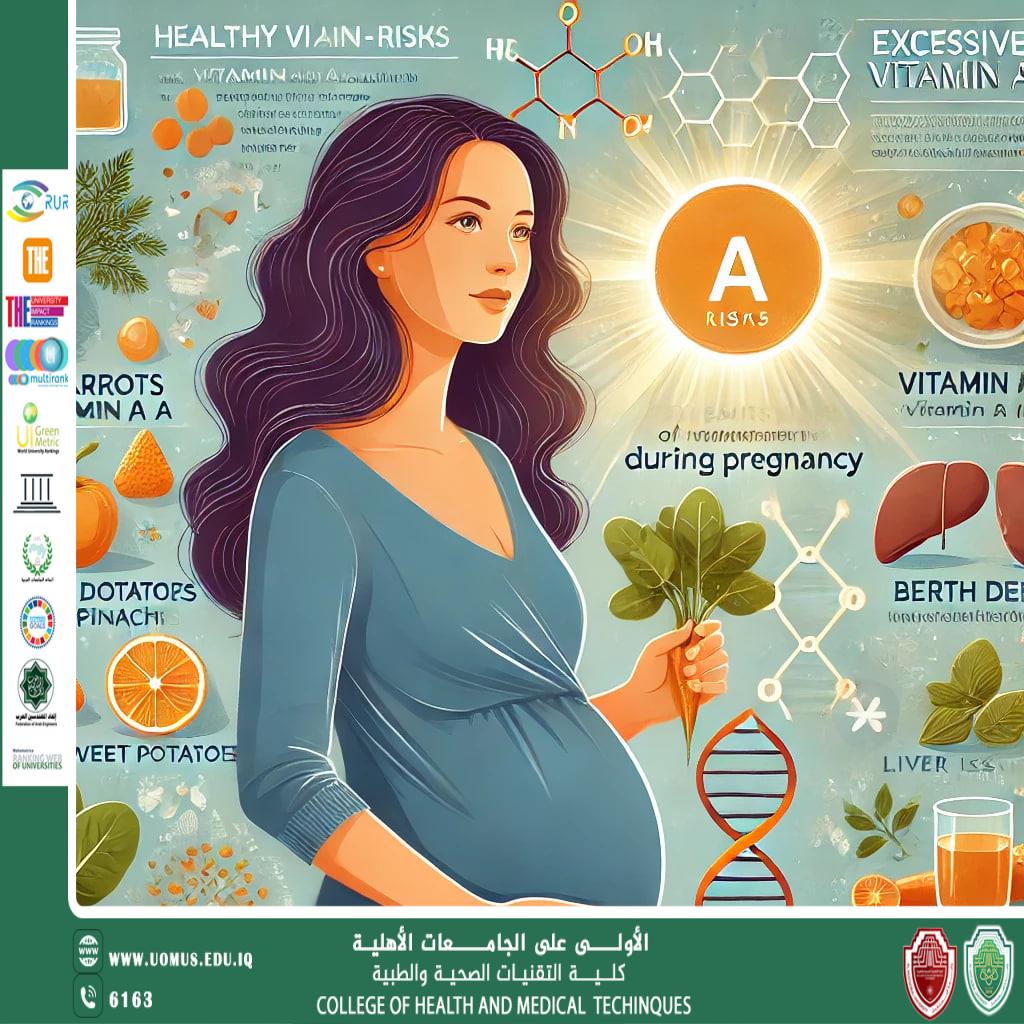
Vitamin A and Pregnancy
Vitamin A is a crucial micronutrient for pregnant women and their fetuses. In addition to being essential for morphological and functional development and for ocular integrity, vitamin A exerts systemic effects on several fetal organs and on the fetal skeleton. Vitamin A requirements during pregnancy are therefore greater. Vitamin A deficiency (VAD) remains the leading cause of preventable blindness in the world. VAD in pregnant women is a public health issue in most developing countries. In contrast, in some developed countries, excessive vitamin A intake during pregnancy can be a concern since, when in excess, this micronutrient may exert teratogenic effects in the first 60 days following conception. Routine prenatal vitamin A supplementation for the prevention of maternal and infant morbidity and mortality is not recommended; however, in regions where VAD is a public health issue, vitamin A supplementation is recommended to prevent night blindness. Given the importance of this topic and the lack of a complete, up-to-date review on vitamin A and pregnancy, an extensive review of the literature was conducted to identify conflicting or incomplete data on the topic as well as any gaps in existing data.<br />The metabolism of vitamin A is complex and involves different forms, sources, and mechanisms such as carrier proteins, enzymes, storage, and physiological and pathological complications. In humans, vitamin A has three active forms (retinal, retinol and retinoic acid) and a form of storage in the liver (retinyl ester). This liposoluble micronutrient is not synthesized by the body and must be obtained through the diet. It is available from two main sources: preformed vitamin A (retinol and retinyl ester) and provitamin A (caratenoids). Of the numerous naturally occurring carotenoids, beta-carotene, alpha carotene, and beta-cryptoxanthin are major provitamin A carotenoids present in foods.<br />Preformed vitamin A is found in foods of animal origin such as dairy products (e.g., milk, yoghurt, and cheese), liver, fish oils, and human milk. Provitamin A, from vegetable sources, is found in fruits, leaves, and tubers such as carrots, pumpkin, kale, spinach, sweet potato, papaya, mango, and red palm oil. Brazilian buriti (Mauritia vinifera) and palm oil (Elaeis guineensis) represent the richest sources of provitamin A in Brazil. The absorption of vitamin A from vegetable sources is considered poor, and foods of animal origin may be necessary to achieve adequate levels in the body.<br />The digestion and absorption of vitamin A are associated with the absorption of lipids. Therefore, critically low dietary fat content (less than 5–10 g/day) or conditions such as pancreatic and hepatic diseases and frequent gastroenteritis that interfere with the digestion or absorption of lipids, resulting in steatorrhea, can interfere with the absorption of vitamin A.<br />With regard to provitamin A, mammals use both carotenoid oxygenases, β-carotene-15,15′-oxygenase (BCO1), and β-carotene-9′,10′-oxygenase (BCO2) to synthesize retinoids from provitamin A carotenoids. Cleavage by BCO2 produces apocaretenoids, which are converted into retinoids by BCO1. Furthermore, β-cryptoxanthin plays an important role in vitamin A production by limiting competition between the metabolites of β-carotene based on the substrate specificity of BCO2 for carotenoids with 3-OH-α-ionone ring sites. This is also evident from the occurrence of β-cryptoxanthin accumulation in BCO2-deficient mice. The retinol absorbed can be released directly into the extrahepatic tissues or captured by the liver, where it can be stored or released back into the bloodstream to meet the body’s requirement. The liver reserve may be able to fulfill the required demands for a long period of time (up to months).<br />In any tissue, including the liver, vitamin A is converted to retinoic acid, which is the active metabolite required for proper morphogenesis. Unlike retinol, retinoic acid is not a stable metabolite, being present in very low levels in serum. High concentrations of certain metabolites of retinoic acid (trans-retinoic acid and 13-cis-retinoic acid) can influence gene activity during critical periods of organogenesis and embryogenesis, leading to teratogenicity.<br />Circulating vitamin A is transported in the plasma in a 1:1 complex with retinol-binding protein (RBP). The retina and other tissues dependent on vitamin A have specific binding sites for RBP and vitamin A. As RBP is the only carrier, conditions that reduce its levels such as proteinuria, kwashiorkor (protein malnutrition), and zinc deficiency may contribute to VAD. For example, pre-eclampsia, which evolves with proteinuria, may cause a decrease in serum retinol levels.<br />The transfer of vitamin A from mother to child occurs via the placenta during gestation and at birth and via the mammary gland during lactation (breastfeeding). During pregnancy, due to the decrease in serum retinol levels in pregnant women (particularly in the third quarter) and the selective placental barrier, the newborn hepatic reserves of vitamin A are low at birth to avoid possible teratogenic effects. After birth, a major part of serum retinol is transported to the breast by RBP, reaching the breast milk. From then on, the transport of vitamin A to breast milk in the first six months of life provides 60-fold more vitamin A when compared with the placental route during the entire pregnancy. Furthermore, breast milk also transports active provitamin A carotenoids, which serve as additional nutrients for the infant. Despite the importance of carotenoids in promoting the health of breast-feeding mothers and their newborns, in recent studies conducted with rats in early life (during breast-feeding), excess vitamin A intake has been associated with obesity.<br /><br />3. Vitamin A Deficiency during Pregnancy: Epidemiological Aspects<br />Despite extensive understanding of the pathophysiology of VAD, with its signs and symptoms being well recognized by health professionals and a proportion of the general population, VAD remains among the major collective health priorities in the world today, together with iron-deficiency anemia and iodine deficiency. Regardless of national and international agreements involving policy makers, program managers in health and education, and multisector programs of action (e.g., agricultural policies, food supply and enrichment of industrialized foods with specific nutrients, and selective distribution of basic food baskets), epidemiological control of VAD remains a challenge in Brazil and in several other developing countries.<br />Regrettably, basic data for the development, implementation, and evaluation and monitoring of policies and programs (public or private) are therefore unavailable at the consistency required to resolve the problem at the population level. For example, and principally as an object of study, the important issue of VAD in pregnant women is without doubt the most obscure link in the chain of epidemiological events related to this specific nutritional deficiency at the national and international level.<br />Pregnancy represents a nutritionally crucial period, either because of previous deficiencies being reduced or aggravated by the gestational process, or because excesses and inadequacies of nutrients in the diet may produce specific nutritional disorders. Thus, nutrients including vitamin A can interfere with the occurrence or worsening of previous or coexisting diseases during pregnancy, childbirth, and in the postpartum.<br />The WHO defines VAD in pregnancy as serum retinol levels of <0.70 µmol/L, with the condition being considered a serious public health issue when the prevalence occurs in 20% or more of pregnant women; moderate when affecting between 10% and 20%; and mild when between 2% and 10%. It is noteworthy that serum retinol levels should ideally be analyzed using high performance liquid chromatography (HPLC).<br /><br /> Conclusions<br />According to current evidence, adequate levels of vitamin A during pregnancy are of critical importance for the health of pregnant women and their fetuses. Unfortunately, to date, VAD in pregnancy is considered a public health issue. In the past decade, few studies have assessed the nutritional status of vitamin A in pregnant Brazilian women, and further studies with new approaches and new designs should be performed to assess the real magnitude of this problem, particularly in developing countries.<br />Previous publications reporting a prevalence of 5.2% [59] and 6.2% [81] for serum retinol levels below 0.70 µmol/L may suggest that VAD in pregnant women could finally be close to coming within epidemiological control. Although this is a promising prospect, in view of its importance in decision-making with regard to the readjustment of policies and management of programs on the issue, it should be re-evaluated in new assessments conducted in accordance with WHO and BRINDA recommendations.<br /><br />د. فرقد صالح<br /><br />AL_mustaqbal University is the first university in Iraq