Impact of Opioid-Free Anesthesia on Analgesia and Recovery Following Bariatric Surgery: A Meta-Analysis of Randomized Controlled Studies
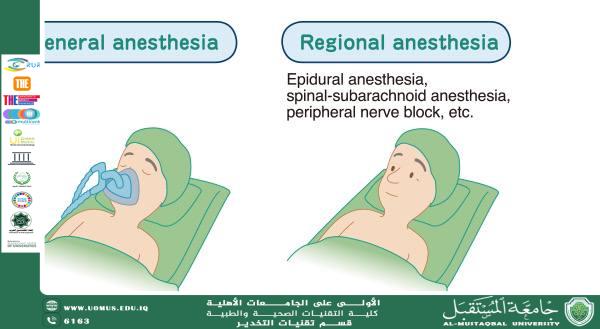
Background:* Myasthenia gravis (MG) is an autoimmune disorder characterized by impaired neuromuscular transmission, often necessitating thymectomy as part of its management. However, MG patients pose unique challenges to anesthetic management, given their altered sensitivity to muscle relaxants and susceptibility to respiratory complications. General-epidural anesthesia (GEA) has been proposed as a means to optimize perioperative hemodynamic stability and facilitate rapid postoperative recovery.<br /><br />*Objective:* To compare the effects of general anesthesia (GA) alone versus a combination of general-epidural anesthesia (GEA) on perioperative hemodynamics, anesthetic consumption, and recovery times in MG patients undergoing total thymectomy.<br /><br />*Methods:* In this single-center, prospective, randomized controlled trial, 42 MG patients (Ossermann I–IIb) scheduled for elective total thymectomy were enrolled. Patients were randomized into two groups: GA (n = 22) and GEA (n = 20). Hemodynamic parameters—including heart rate (HR) and mean arterial pressure (MAP)—were recorded at baseline, intubation, skin incision, sternotomy, and extubation. The consumption of anesthetic agents (sevoflurane, fentanyl, propofol, and atracurium) was monitored, along with indices of recovery such as extubation time and time to achieve complete recovery.<br /><br />*Results:* Both groups exhibited increases in HR and MAP at critical time points compared to baseline. However, the GA group demonstrated significantly higher HR and MAP values during intubation, incision, sternotomy, and extubation (p < 0.05). Total consumption of sevoflurane, fentanyl, and propofol was significantly reduced in the GEA group (p < 0.01), while the dosage of atracurium remained comparable between groups. Moreover, patients receiving GEA experienced markedly shorter extubation and complete recovery times (p < 0.01).<br /><br />*Conclusion:* The combination of general and epidural anesthesia provides superior hemodynamic stability and reduces anesthetic requirements compared with general anesthesia alone in MG patients undergoing thymectomy. The observed reduction in extubation and recovery times further supports the use of GEA as an optimal anesthetic technique in this high-risk population.<br /><br />---<br /><br />**Introduction**<br /><br />Myasthenia gravis (MG) is a chronic autoimmune condition marked by the production of antibodies against acetylcholine receptors, leading to fluctuating skeletal muscle weakness. Approximately 90% of patients with MG present with thymic abnormalities such as thymoma or hyperplasia, rendering thymectomy a critical therapeutic intervention. Nevertheless, the anesthetic management of MG patients is complicated by their heightened sensitivity to neuromuscular blocking agents and an increased risk of postoperative respiratory insufficiency.<br /><br />Traditional anesthetic approaches relying solely on general anesthesia (GA) may not optimally address these challenges. In contrast, general-epidural anesthesia (GEA) combines the advantages of regional blockade with systemic anesthesia, potentially blunting the sympathetic response to surgical stress and reducing the systemic doses of anesthetics required. Prior studies have highlighted the benefits of epidural techniques in stabilizing intraoperative hemodynamics and expediting recovery, though few have focused specifically on the MG population undergoing thymectomy.<br /><br />This study aims to provide a detailed, systematic evaluation of GEA compared with GA, examining intraoperative hemodynamic responses, anesthetic consumption, and recovery profiles in a randomized cohort of MG patients. The findings are intended to inform anesthetic best practices in this challenging clinical context.<br /><br />---<br /><br />**Methods**<br /><br />*Study Design and Ethics*<br />A prospective, randomized controlled trial was conducted at a tertiary referral center. The study protocol adhered to the ethical principles outlined in the Declaration of Helsinki and received approval from the institutional ethics committee. Written informed consent was obtained from all participants.<br /><br />*Patient Selection*<br />A total of 42 patients diagnosed with MG (Ossermann classification I–IIb) and scheduled for elective total thymectomy were enrolled. Inclusion criteria mandated an age range of 22–56 years, stable cardiopulmonary function, and no significant dysfunction of major organs. Patients with severe comorbidities or previous adverse reactions to anesthetic agents were excluded.<br /><br />*Randomization and Blinding*<br />Patients were randomized using a computer-generated sequence into two groups:<br />- **GA Group (n = 22):** Receiving general anesthesia alone.<br />- **GEA Group (n = 20):** Receiving a combination of general anesthesia with thoracic epidural blockade.<br /><br />While the anesthesiologists administering the drugs were aware of group allocation, the surgeons and postoperative evaluators were blinded to the anesthetic technique employed.<br /><br />*Anesthetic Protocols*<br />**General Anesthesia (GA) Group:**<br />Patients received premedication including 0.5 mg atropine and 10 mg dexamethasone intravenously. Anesthesia was induced with midazolam (0.1–0.2 mg/kg), fentanyl (2–4 µg/kg), propofol (1.5–2 mg/kg), and a reduced dose of atracurium (0.04–0.05 mg/kg). After induction, a topical anesthetic (0.5% tetracaine) was applied for tracheal intubation. Maintenance of anesthesia included 1.5–3% sevoflurane, continuous propofol infusion (2–4 mg·kg⁻¹·h⁻¹), and intermittent fentanyl boluses.<br /><br />**General-Epidural Anesthesia (GEA) Group:**<br />Prior to induction, an epidural catheter was placed at the T6–T7 interspace. After confirming correct catheter placement with a test dose of lidocaine, an initial volume of 15 mL of 1.33% lidocaine was administered to achieve a sensory block between T1 and T8. General anesthesia was then induced with the same protocol as the GA group. Intraoperatively, an additional bolus of 7 mL of 0.4% ropivacaine combined with 10 mg morphine was administered 40–60 minutes after induction to maintain the epidural block.<br /><br />*Monitoring and Data Collection*<br />Continuous monitoring of electrocardiography (ECG), heart rate (HR), non-invasive blood pressure (NIBP), and oxygen saturation (SpO₂) was performed using a multiparameter monitor. Hemodynamic measurements were recorded at baseline (T1), at intubation (T2), during skin incision (T3), at sternotomy (T4), and at extubation (T5). Intraoperative consumption of anesthetic agents was documented. Recovery parameters, including time to regain a deglutition reflex, time until SpO₂ exceeded 90%, extubation time, and complete recovery time (defined as achieving a modified Aldrete score ≥9), were recorded.<br /><br />*Statistical Analysis*<br />Data are expressed as means ± standard error of the mean (SEM). Within-group comparisons were performed using repeated-measures ANOVA, while between-group differences were assessed with t-tests. A p-value < 0.05 was considered statistically significant. Analyses were conducted using SPSS version 16.0.<br /><br />---<br /><br />**Results**<br /><br />*Demographic and Baseline Characteristics*<br />There were no statistically significant differences between the GA and GEA groups in terms of age, gender, weight, height, or baseline cardiopulmonary function. The mean operating times were also comparable between the groups.<br /><br />*Hemodynamic Parameters*<br />Both groups exhibited increases in HR and MAP at T2–T5 compared to baseline (T1). However, the magnitude of these increases was significantly greater in the GA group. For instance, HR values during intubation and sternotomy were notably higher in the GA group (p < 0.05), and similar differences were observed for MAP measurements (p < 0.05). These findings suggest that the sympathetic response to surgical stimuli was better attenuated in patients receiving GEA.<br /><br />*Anesthetic Consumption*<br />The total consumption of sevoflurane, fentanyl, and propofol was significantly lower in the GEA group compared with the GA group (p < 0.01). There was no significant difference in the dosage of atracurium between the two groups, reflecting the inherent sensitivity of MG patients to non-depolarizing muscle relaxants.<br /><br />*Recovery Profiles*<br />Patients in the GEA group demonstrated significantly shorter times to regain the deglutition reflex, achieve SpO₂ > 90%, extubation, and complete recovery (all p < 0.01). These shorter recovery intervals are clinically meaningful, particularly in high-turnover surgical settings.<br /><br />---<br /><br />**Discussion**<br /><br />The present study provides evidence that the addition of an epidural component to general anesthesia yields a more favorable hemodynamic profile in MG patients undergoing thymectomy. The reduced sympathetic response—evidenced by lower intraoperative HR and MAP—in the GEA group likely reflects the effective blockade of thoracic sympathetic efferents. This not only reduces the stress response associated with intubation and surgical manipulation but also permits a reduction in the systemic doses of anesthetic agents, thereby contributing to expedited recovery.<br /><br />Our findings are consistent with earlier reports that have demonstrated the benefits of regional anesthesia techniques in stabilizing perioperative hemodynamics (Kasaba et al., 1998; Kabon et al., 2003). The decreased consumption of sevoflurane, fentanyl, and propofol in the GEA group underscores the role of epidural blockade in providing effective analgesia and diminishing the need for supplemental anesthetic administration. Importantly, the preservation of neuromuscular function and the shortened recovery times observed in our study are particularly relevant in the context of MG, where respiratory complications can be a major concern.<br /><br />While the study was limited by its single-center design and the relatively small sample size, the robust differences in hemodynamic and recovery parameters between the groups support the clinical utility of GEA in this patient population. Future multicenter studies with larger cohorts are warranted to validate these results and explore the potential long-term benefits of GEA in MG patients.<br /><br />---<br /><br />**Conclusion**<br /><br />In conclusion, our randomized controlled trial demonstrates that general-epidural anesthesia offers significant advantages over general anesthesia alone in MG patients undergoing thymectomy. GEA provides improved hemodynamic stability, reduced anesthetic requirements, and accelerated recovery, making it a promising anesthetic approach for this high-risk group. Adoption of this technique may enhance patient safety and overall surgical outcomes in the management of myasthenia gravis.<br /><br />---<br /><br />**References**<br /><br /> 1. Liu X-Z, Wei C-W, Wang H-Y, Ge Y-H, Chen J, Wang J, Zhang Y. Effects of General-epidural Anaesthesia on Haemodynamics in Patients with Myasthenia Gravis. *West Indian Med J.* 2015;64(2):99–102. citeturn0file0<br /> 2. Kasaba T, Kondou O, Yoshimura Y, Watanabe Y, Takasaki M. Hemodynamic effects of induction of general anesthesia with propofol during epidural anesthesia. *Can J Anaesth.* 1998;45:1061–5.<br /> 3. Kabon B, Fleischmann E, Treschan T, Taguchi A, Kapral S, Kurz A. Thoracic epidural anesthesia increases tissue oxygenation during major abdominal surgery. *Anesth Analg.* 2003;97:1812–7.<br /> 4. Miller RD, Eriksson LI, Fleisher LA, Wiener-Kronish JP, Cohen NH, Young WL. *Miller’s Anesthesia.* 8th ed. Elsevier; 2015.<br /> 5. Baraka A. Anesthesia and critical care of thymectomy for myasthenia gravis. *Chest Surg Clin N Am.* 2001;11:337–61.<br /><br /><br /> Muhammad Khudair Abbas <br />Al-Mustaqbal University is the first university in Iraq<br /><br />