Leishmaniasis
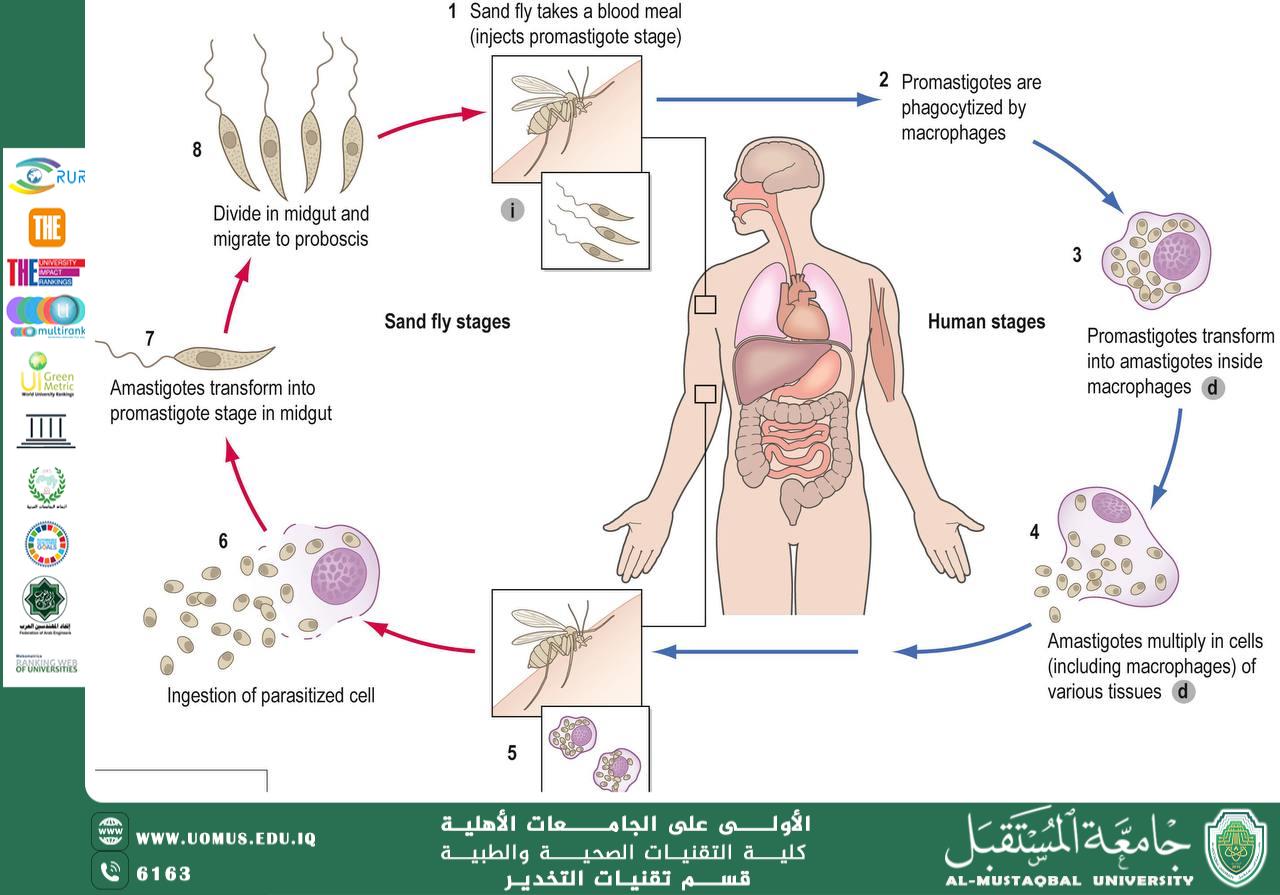
<br />Leishmaniasis is caused by a protozoa parasite from over 20 Leishmania species. Over 90 sandfly species are known to transmit Leishmania parasites. There are 3 main forms of the disease:<br /><br />Visceral leishmaniasis (VL), also known as kala-azar, is fatal if left untreated in over 95% of cases. It is characterized by irregular bouts of fever, weight loss, enlargement of the spleen and liver, and anaemia. Most cases occur in Brazil, east Africa and India. An estimated 50 000 to 90 000 new cases of VL occur worldwide annually, with only 25–45% reported to WHO. It has outbreak and mortality potential. <br /><br />Cutaneous leishmaniasis (CL) is the most common form and causes skin lesions, mainly ulcers, on exposed parts of the body. These can leave life-long scars and cause serious disability or stigma. About 95% of CL cases occur in the Americas, the Mediterranean basin, the Middle East and central Asia. It is estimated that 600 000 to 1 million new cases occur worldwide annually but only around 200 000 are reported to WHO.<br /><br />Mucocutaneous leishmaniasis leads to partial or total destruction of mucous membranes of the nose, mouth and throat. Over 90% of mucocutaneous leishmaniasis cases occur in Bolivia (the Plurinational State of), Brazil, Ethiopia and Peru.<br /><br />Danyah Baiee, [19/03/2025 9:31 AM]<br />Transmission<br />Leishmania parasites are transmitted through the bites of infected female phlebotomine sandflies, which feed on blood to produce eggs. Some 70 animal species, including humans, can be the source of Leishmania parasites.<br /><br /><br />Major risk factors<br /><br />Socioeconomic conditions<br /><br />Poverty increases the risk for leishmaniasis. Poor housing and domestic sanitary conditions (lack of waste management or open sewerage) may increase sandfly breeding and resting sites, as well as their access to humans. Sandflies are attracted to crowded housing because it is easier to bite people and feed on their blood. Human behaviour, such as sleeping outside or on the ground, may increase risk.<br /><br />Malnutrition<br /><br />Diets lacking protein-energy, iron, vitamin A and zinc increase the risk that an infection will progress to a full-blown disease.<br /><br />Population mobility<br /><br />Epidemics of leishmaniasis often occur when many people who are not immune move into areas where the transmission is high. <br /><br />Environmental and climate changes<br /><br />The incidence of leishmaniasis can be affected by changes in urbanization, deforestation or the human incursion into forested areas.<br />Climate change is affecting the spread of leishmaniasis though changes in temperature and rainfall, which affect the size and geographic distribution of sandfly populations. Drought, famine and flood also cause migration of people into areas where the transmission of the parasite is high.<br /><br />Diagnosis and treatment<br /><br />People suspected of suffering from visceral leishmaniasis should seek medical care immediately. In visceral leishmaniasis, diagnosis is made by combining clinical signs with parasitological or serological tests (such as rapid diagnostic tests). In cutaneous and mucocutaneous leishmaniasis serological tests have limited value and clinical manifestation with parasitological tests confirms the diagnosis.<br />The treatment of leishmaniasis depends on several factors including type of disease, concomitant pathologies, parasite species and geographic location. Leishmaniasis is a treatable and curable disease, which requires an immunocompetent system because medicines will not get rid of the parasite from the body, thus the risk of relapse if immunosuppression occurs. All patients diagnosed with visceral leishmaniasis require prompt and complete treatment<br /><br />Prevention and control<br /><br />Preventing and controlling the spread of leishmaniasis is complex and requires many tools. Key strategies include:<br />Early diagnosis and effective prompt treatment reduce the prevalence of the disease and prevents disabilities and death. It helps to reduce transmission and to monitor the spread and burden of disease. There are highly effective and safe anti-leishmanial medicines particularly for visceral leishmaniasis, although they can be difficult to use. Access to medicines has significantly improved thanks to a WHO-negotiated price scheme and a medicine donation programme through WHO.<br />Vector control helps to reduce or interrupt transmission of disease by decreasing the number of sandflies. Control methods include insecticide spray, use of insecticide-treated nets, environmental management and personal protection.<br />Effective disease surveillance is important to promptly monitor and act during epidemics and situations with high case fatality rates under treatment.<br />Control of animal reservoir hosts is complex and should be tailored to the local situation.<br />Social mobilization and strengthening partnerships – mobilization and education of the community with effective behavioural change interventions must always be locally adapted. Partnership and collaboration with various stakeholders and other vector-borne disease control programmes is critical.<br /><br />م.دانيه عادل<br /><br />Al-Mustaqbal University is the first university in Iraq<br />