An article by the lecturer Hassan Abd Ali entitled(Amblyopia in Children: Current Understanding and Management)
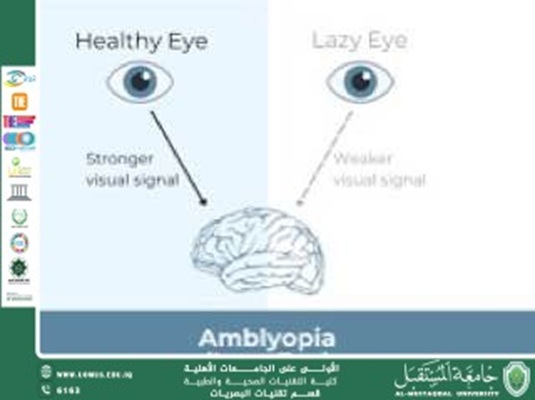
Amblyopia in Children: Current Understanding and Management<br /><br />Introduction<br />Amblyopia, commonly known as “lazy eye,” is the most frequent cause of visual impairment in children, affecting approximately 2–3% of the pediatric population. It is characterized by reduced visual acuity in one or occasionally both eyes, not attributable to any structural abnormality of the eye or visual pathways. Early diagnosis and intervention are critical, as untreated amblyopia can result in permanent visual deficits.<br /><br />Etiology and Risk Factors<br />The primary causes of amblyopia include strabismus (strabismic amblyopia), significant refractive errors (refractive amblyopia), and form deprivation (deprivation amblyopia).<br /> • Strabismic amblyopia occurs when misalignment of the eyes leads the brain to suppress input from one eye to avoid double vision.<br /> • Refractive amblyopia arises from uncorrected anisometropia or high bilateral refractive errors, leading to chronic blurred vision in one or both eyes.<br /> • Deprivation amblyopia results from conditions that obstruct visual input, such as congenital cataracts or ptosis.<br />Risk factors include a family history of amblyopia, premature birth, low birth weight, and developmental disabilities.<br /><br />Pathophysiology<br />Amblyopia results from disrupted visual development during the critical period, typically the first seven years of life. Abnormal visual experience leads to altered neural connections within the primary visual cortex, with subsequent suppression of the affected eye’s input.<br /><br />Diagnosis<br />Early detection through vision screening is essential. Diagnosis relies on a comprehensive eye examination, including assessment of visual acuity, ocular alignment, refractive error, and ocular health. Techniques like preferential looking tests, fixation preference, and modern objective screening tools (e.g., photoscreening) have improved early diagnosis.<br /><br />Management and Treatment<br />The cornerstone of amblyopia treatment is promoting use of the amblyopic eye to strengthen visual pathways. Management strategies include:<br /> • Optical correction: Full-time correction of refractive errors with glasses or contact lenses is the first step.<br /> • Occlusion therapy: Patching the dominant eye for prescribed hours per day to force use of the amblyopic eye.<br /> • Pharmacologic penalization: Use of atropine drops in the better-seeing eye to blur vision and stimulate use of the amblyopic eye.<br /> • Vision therapy: Recent studies suggest that binocular training and digital therapies may enhance outcomes by improving binocular function and reducing suppression.<br /> • Surgical intervention: In cases of strabismus, surgical alignment may be necessary either before or during amblyopia therapy.<br /><br />Prognosis<br />The earlier amblyopia is diagnosed and treated, the better the visual prognosis. While treatment is most effective in children under the age of 7, emerging evidence supports the potential for visual improvement in older children and even adolescents with structured therapy.<br /><br />Recent Advances<br />Recent research emphasizes the importance of binocular approaches rather than traditional monocular therapies. Video games, virtual reality systems, and interactive digital therapies are currently under investigation and show promising results in promoting binocular visual function alongside monocular improvement.<br /><br />Conclusion<br />Amblyopia remains a significant pediatric visual health issue, but with early detection and comprehensive treatment strategies, most children can achieve substantial visual improvement. Advances in understanding the neuroplasticity of the visual system continue to inspire innovative therapeutic approaches, offering hope for better outcomes across a broader age range.<br /><br />References<br /> 1. Levi, D. M., & Li, R. W. (2020). Perceptual learning as a potential treatment for amblyopia: A review. Vision Research, 176, 118–129.<br /> 2. Holmes, J. M., & Clarke, M. P. (2020). Amblyopia. The Lancet, 396(10264), 134–146.<br /> 3. Birch, E. E. (2022). Amblyopia and binocular vision.<br /><br />“Al-Mustaqbal University is the top-ranked among private universities.”<br />