A scientific article by the lecturer, Assist.Lect. Ali Hadi Al-Husseini (Tear Fluid Analysis in the Early Diagnosis of Ocular Inflammatory and Immune Disorders)
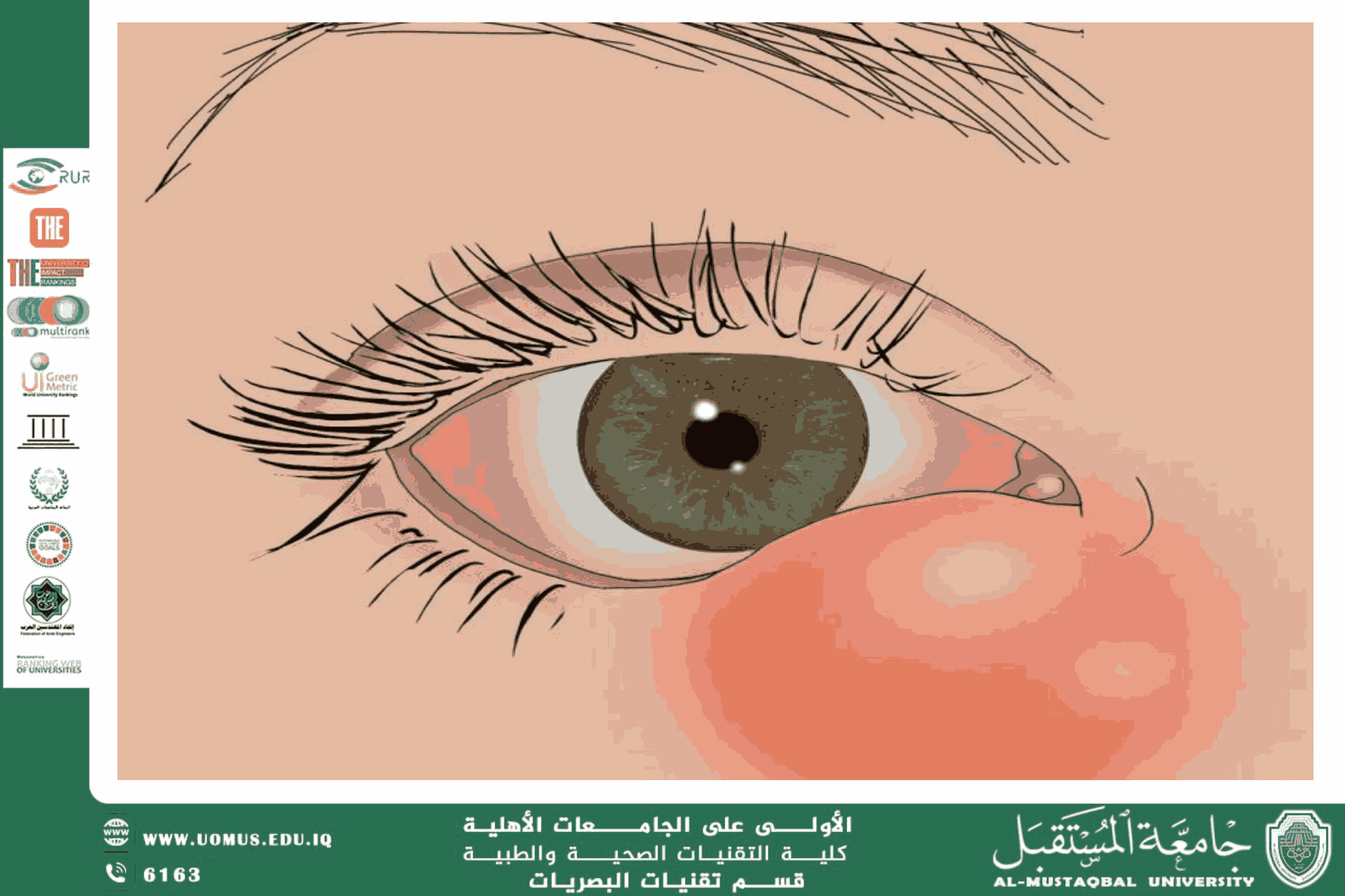
Tear fluid is essential for ocular surface homeostasis, providing not only lubrication for the cornea and conjunctiva but also containing a complex mixture of proteins, antibodies, and enzymes that reflect the immune status of both the eye and the systemic body. Therefore, analyzing tear components has emerged as a significant tool for the early diagnosis of inflammatory and immune-mediated ocular diseases, including chronic conjunctivitis, Sjögren’s syndrome, and autoimmune ocular inflammation.<br />Biochemical Composition and Significance<br />Tear fluid contains:<br />• Antibodies (IgA, IgG) indicating local or systemic immune responses.<br />• Antimicrobial enzymes (Lysozyme, Lactoferrin) that protect against bacterial and fungal infections.<br />• Inflammatory cytokines (IL-1, IL-6, TNF-α) which reflect active inflammation.<br />Clinical Applications<br />1. Sjögren’s Syndrome: Reduced lactoferrin levels combined with elevated inflammatory cytokines in tears may serve as an early biomarker before clinical dry eye manifestations appear.<br />2. Chronic Immune-Mediated Conjunctivitis: Tear cytokine and antibody profiling can help determine disease severity and monitor therapeutic response.<br />3. Therapeutic Monitoring: Tracking changes in tear composition provides a non-invasive method to assess the efficacy of topical and systemic immune-modulating treatments.<br />Tear fluid is not merely a lubricating medium for the eye; it represents a precise diagnostic window into inflammatory and immune ocular disorders. Integrating tear analysis into early diagnostic protocols can significantly enhance patient care and reduce vision-threatening complications associated with chronic ocular inflammation.<br />