The Relationship Between Serum Levels of Vitamin D, CD34, CD133, Iron, and Zinc and Their Association with Diabetic Nephropathy in Patients with Type 2 Diabetes Mellitus Asst. Prof. Dr. Muslim Mohammed Mousa
Introduction
Diabetic nephropathy (DN) is one of the major microvascular complications of type 2 diabetes mellitus (T2DM) and is considered a leading cause of chronic kidney disease (CKD) worldwide. This condition arises due to chronic hyperglycemia and the accompanying imbalance in cellular oxidation–reduction processes within kidney cells, leading to the accumulation of reactive oxygen species (ROS) and gradual damage to the glomerular capillaries. Consequently, this results in a decline in the glomerular filtration rate (GFR) and deterioration of kidney function.
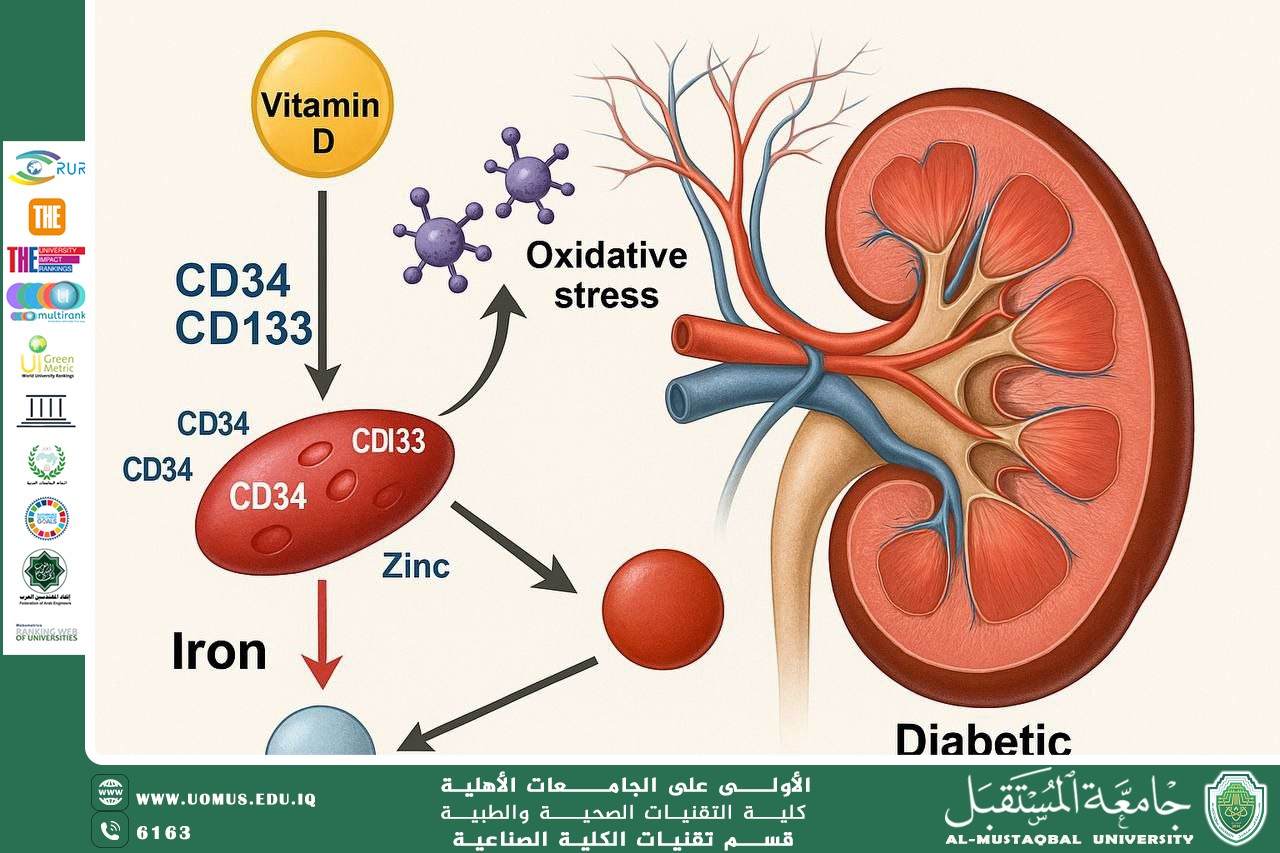
Understanding the relationship between oxidative stress biomarkers and cellular factors affecting vascular integrity in the kidney is an important step toward early detection of the initial stages of diabetic nephropathy. Among these indicators, Vitamin D plays a fundamental role in regulating glucose metabolism and immunity, while the trace elements iron and zinc directly influence the activity of antioxidant enzymes. Additionally, vascular progenitor stem cells, identified by the markers CD34 and CD133, serve as vital indicators of the body’s capacity for vascular repair.
Recent studies indicate that decreased levels of Vitamin D, CD34, and CD133 reflect impaired angiogenesis and vascular repair mechanisms in diabetic patients. Elevated serum iron, on the other hand, promotes free radical formation through Fenton reactions, exacerbating oxidative damage in kidney cells. Zinc is an essential element in the structure of antioxidant enzymes such as Superoxide Dismutase (SOD) and Glutathione Peroxidase (GPx), playing a key role in membrane stability and reducing the effects of oxidative stress.
This study aims to evaluate the relationship between serum levels of Vitamin D, CD34, CD133, iron, and zinc, and their association with the severity of diabetic nephropathy in patients with type 2 diabetes mellitus, to assess their potential as auxiliary diagnostic markers or indicators for disease severity and progression.
The study results showed that diabetic patients with nephropathy had significantly lower levels of Vitamin D, CD34, and CD133 compared to those without nephropathy, while serum iron levels were markedly elevated. No statistically significant differences were observed in zinc levels. These findings suggest that imbalances in mineral and vitamin levels, along with impaired vascular stem cell repair capacity, contribute to increased oxidative stress and kidney function deterioration.
Furthermore, elevated iron and decreased Vitamin D, CD34, and CD133 levels correlated with the severity of diabetic nephropathy, making them important diagnostic and predictive biomarkers. Regulating these elements through nutrition or pharmacological intervention, alongside blood glucose control, may help reduce complications and delay the progression of renal failure.
Adopting these markers in clinical assessment could support the implementation of precision medicine in diagnosing and treating diabetic nephropathy through personalized therapeutic plans tailored to each patient’s molecular profile, thereby reducing disease burden and improving patients’ quality of life.
Al-Mustaqbal University – The First University in Iraq