Bronchospasm – Scientific Article
Introduction
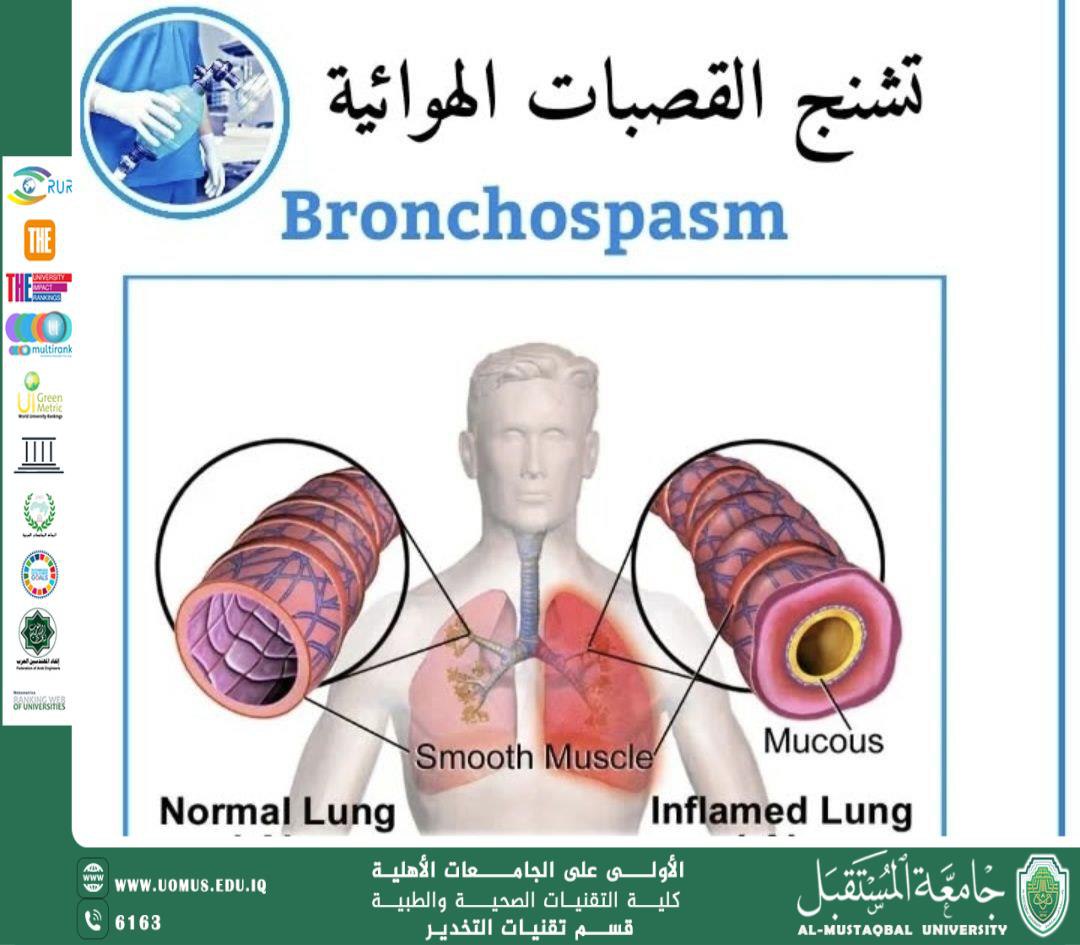
Bronchospasm is defined as a sudden, involuntary contraction of the smooth muscles surrounding the bronchi, resulting in airway narrowing and reduced airflow to and from the lungs. It is a common and potentially serious condition, especially in patients with asthma, allergies, chronic smokers, and individuals undergoing general anesthesia.
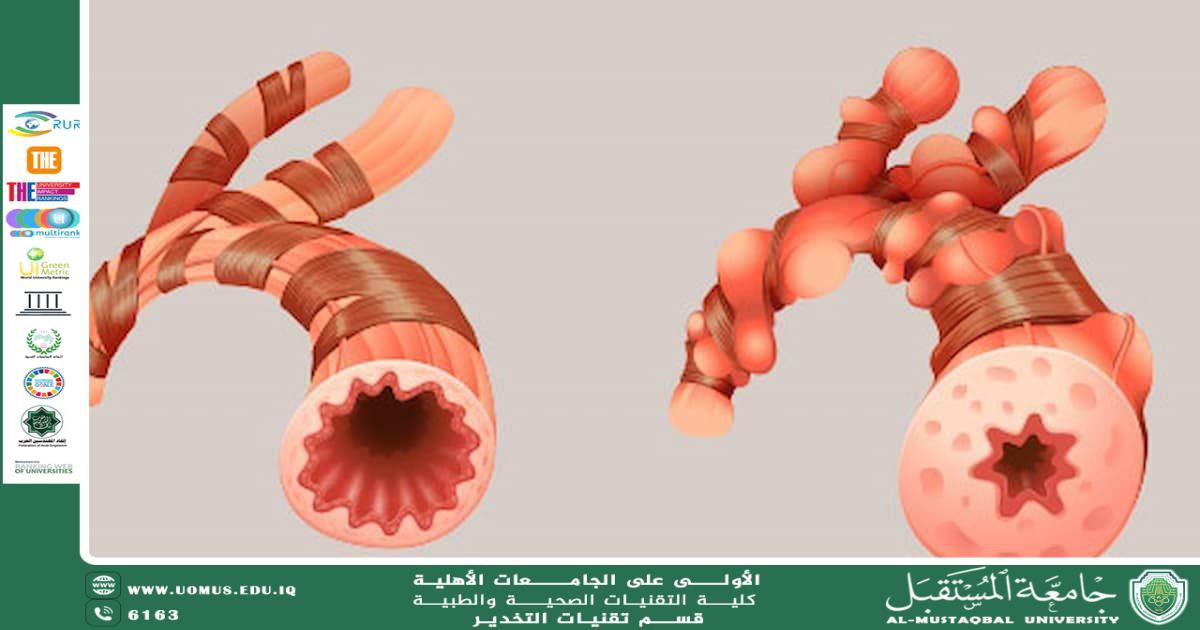
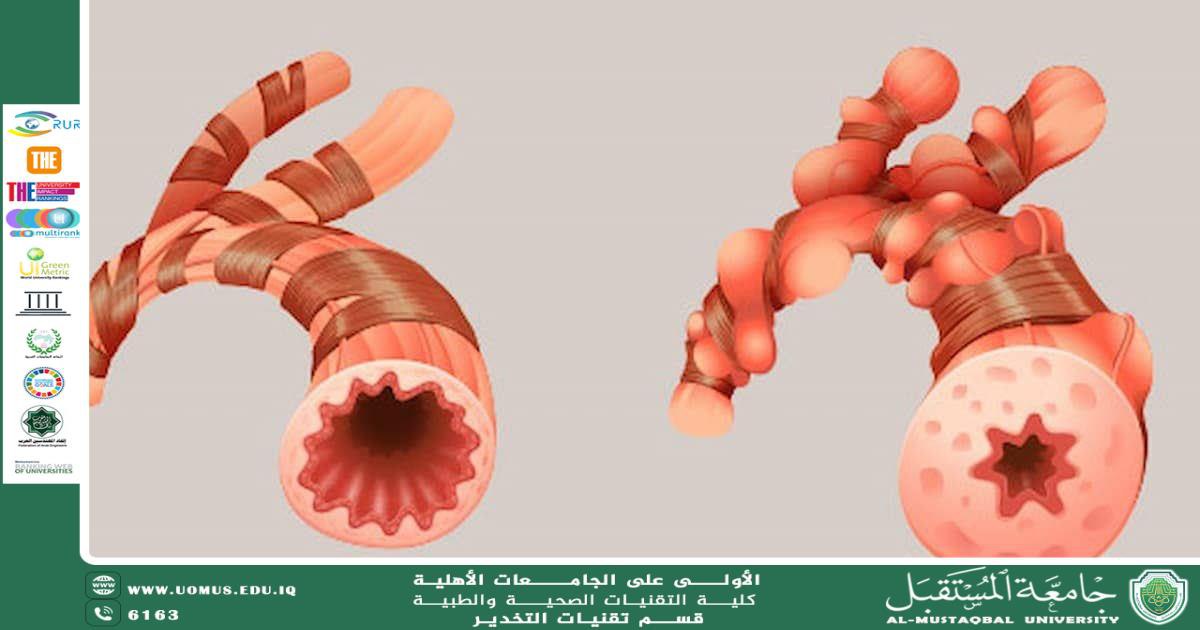
Pathophysiology
Bronchospasm occurs as a result of an inflammatory or allergic response that leads to:
1. Contraction of bronchial smooth muscles,
triggered by the release of mediators such as histamine, leukotrienes, and prostaglandins.
2. Mucosal edema of the bronchial lining.
3. Increased production of thick mucus within the airways.
Collectively, these mechanisms lead to:
• Narrowing of the airway lumen
• Increased airway resistance
• Reduced ventilation
• Difficulty in inhalation and exhalation
Etiology
1. General Respiratory Causes
• Asthma
• Chronic Obstructive Pulmonary Disease (COPD)
• Viral and bacterial respiratory infections
• Exposure to dust, smoke, and strong odors
• Strenuous physical activity
2. Allergic Triggers
• Medications (NSAIDs, beta-blockers, certain antibiotics)
• Pollen
• Animal dander
• Food allergens
3. Anesthesia-Induced Bronchospasm
Important in anesthesia practice, it may result from:
• Light or inadequate anesthesia
• Allergic reactions to anesthetic agents
• Airway irritation due to: suctioning, intubation, extubation, excessive secretions
• Uncontrolled asthma
• Chronic smoking
Clinical Features
Symptoms
• Sudden shortness of breath
• Chest tightness
• Severe coughing
• Wheezing
Signs
• Rapid, shallow breathing
• Difficulty with both inspiration and expiration
• Low oxygen saturation
• Audible wheezing on auscultation
• High peak airway pressures during anesthesia
Diagnosis
• Clinical examination and detection of wheezing
• Pulse oximetry
• Spirometry
• Arterial Blood Gas (ABG) analysis in severe cases
• Observing increased airway pressure on the anesthesia machine
Management
1. Bronchodilators
• Salbutamol (Ventolin): first-line therapy
• Ipratropium bromide
• Epinephrine in severe cases
2. Steroids
• Hydrocortisone
• Dexamethasone
To reduce inflammation and prevent recurrence.
3. Oxygen Therapy
To improve oxygen saturation and prevent hypoxemia.
4. In Anesthesia
• Deepening anesthesia (e.g., Propofol)
• Using Sevoflurane for its bronchodilatory effect
• Suctioning secretions
• Ensuring no tube kinking or obstruction
• IV bronchodilators when needed
Complications
Untreated bronchospasm may lead to:
• Hypoxemia
• Hypercapnia
• Apnea
• Respiratory failure
• Cardiac arrest in severe cases
Prevention
For Patients
• Adequate asthma control
• Avoidance of irritants (smoke, dust)
• Regular use of prescribed inhalers
In Anesthesia
• Preoperative respiratory assessment
• Administering bronchodilators when indicated
• Minimizing airway irritation
• Using appropriate drugs for allergic patients
Conclusion
Bronchospasm is a potentially life-threatening condition, especially in asthmatic patients or during general anesthesia. Early recognition, accurate diagnosis, and prompt management are essential to prevent complications and ensure patient safety.
Hasan Najeh
Al-Mustaqbal University
The First University in Iraq.