Scientific Article by Lecturer Gaith Ali Mahmood : Keratoconus
Introduction
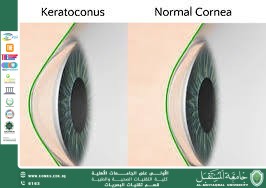
Keratoconus is a progressive degenerative disorder of the cornea, in which the corneal tissue becomes thinner and gradually changes from its normal spherical shape into an irregular cone-like structure. This alteration in shape leads to abnormal light refraction inside the eye, resulting in visual distortions such as blurred vision, double vision, or increased sensitivity to light. The condition typically begins during adolescence or the early twenties and may stabilize in some individuals or continue to progress over time.
Epidemiology
The prevalence of keratoconus ranges from 1 to 5 cases per 2,000 people, though rates may be higher in certain regions due to genetic or environmental factors. The condition affects both males and females, although some studies suggest a slightly higher prevalence in males. Higher incidence is also observed in populations with consanguineous marriages or a family history of the disease.
Causes and Contributing Factors
Although no single definitive cause has been identified, several factors are associated with the development of keratoconus, including:
Genetic predisposition: Research indicates a hereditary component to the disease.
Chronic eye rubbing: Persistent friction may weaken corneal collagen fibers.
Associated conditions: Such as asthma, eczema, Down syndrome, and Marfan syndrome.
Corneal enzymatic imbalance: Certain biochemical changes may increase tissue degradation.
Clinical Symptoms
Symptoms vary depending on the severity of the condition and may include:
Gradual visual blurring
Frequent changes in eyeglass or contact lens prescriptions
Double vision or ghosting
Halos around lights, especially at night
Increased light sensitivity (photophobia)
Headaches related to visual strain
Diagnostic Methods
Diagnosis of keratoconus typically involves several examinations, most notably:
Corneal topography to detect conical shape changes
Pachymetry to measure corneal thickness
Slit-lamp examination to assess structural corneal changes
Refraction tests and visual quality analysis
Disease Stages
Keratoconus can be classified into several stages according to severity:
Mild: Slight visual distortion, managed with glasses or soft lenses
Moderate: Requires rigid gas-permeable or hybrid lenses
Advanced: Significant vision loss requiring surgical intervention
Severe: May necessitate full corneal transplantation
Treatment Options
The treatment plan depends on the stage at diagnosis:
Early stages: Eyeglasses or soft contact lenses
Rigid gas-permeable or hybrid lenses: To compensate for the irregular corneal surface
Corneal Cross-Linking (CXL): A modern procedure using UV light and riboflavin to strengthen corneal collagen fibers
Intracorneal ring segments (Intacs): Used to reshape the cornea
Corneal transplantation: A last-resort option for advanced cases, including partial or full grafts
Recent Advances
Significant progress has been made in the management of keratoconus, including:
Enhanced CXL techniques (such as epithelium-on “Epi-on” procedures)
Improved scleral and hybrid lenses offering superior vision and comfort
Use of artificial intelligence to analyze disease progression and predict future stages
Ongoing clinical trials for genetic and biological therapies aimed at corneal remodeling and tissue regeneration