Liver Failure
Liver failure is a serious medical condition resulting from the loss of the liver’s ability to perform its vital functions, leading to metabolic, immunological, and coagulation disturbances that may be life-threatening. Liver failure may occur in acute or chronic forms, with differing causes, pathophysiological mechanisms, and treatment strategies depending on the pattern of onset. This article aims to review the types of liver failure, its causes, pathophysiology, clinical manifestations, diagnostic methods, and therapeutic options.
Introduction
The liver is one of the most important organs in the human body, playing a central role in metabolism, detoxification, protein synthesis, and regulation of coagulation factors. Severe or progressive damage to hepatocytes leads to impairment of these functions, adversely affecting multiple body systems. Liver failure represents a major clinical challenge due to its high morbidity and mortality rates.
Types of Liver Failure
1. Acute Liver Failure (ALF)
Acute liver failure develops over a short period (days to weeks) in patients without pre-existing liver disease. It is characterized by the rapid onset of hepatic encephalopathy and coagulation abnormalities.
2. Chronic Liver Failure
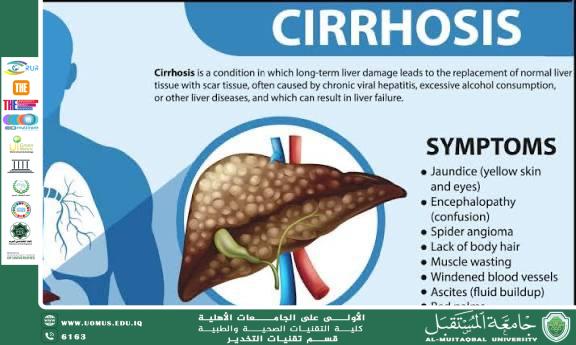
Chronic liver failure results from a gradual deterioration of liver function, most commonly due to liver cirrhosis. It progresses over a long period and is often accompanied by episodes of acute decompensation.
3. Acute-on-Chronic Liver Failure (ACLF)
This condition occurs in patients with underlying chronic liver disease who experience an acute deterioration, and it is associated with a high mortality rate.
Causes of Liver Failure
• Viral infections: such as hepatitis B and C
• Drug-induced toxicity: especially paracetamol (acetaminophen) overdose
• Chronic alcohol consumption
• Autoimmune liver diseases
• Inherited metabolic disorders such as Wilson’s disease
• Hepatic ischemia (shock, heart failure)
Pathophysiology
Liver failure results from extensive hepatocellular necrosis or replacement of functional liver tissue with fibrotic tissue, leading to:
• Reduced synthesis of albumin and coagulation factors
• Accumulation of toxins such as ammonia
• Impaired regulation of glucose and lipid metabolism
• Dysfunction of the immune system
These changes result in systemic complications affecting the brain, kidneys, and circulatory system.
Clinical Manifestations
• Jaundice
• Hepatic encephalopathy (altered level of consciousness)
• Bleeding tendency and easy bruising
• Ascites and peripheral edema
• Nausea and loss of appetite
• General fatigue and weight loss
Diagnosis
Diagnosis is based on:
• Laboratory investigations: elevated liver enzymes, increased bilirubin levels, prolonged prothrombin time
• Imaging studies: ultrasound and computed tomography
• Liver biopsy in selected cases
• Disease severity assessment using scoring systems such as Child-Pugh and MELD scores
Treatment
Supportive Management
• Correction of fluid and electrolyte imbalances
• Management of hepatic encephalopathy (lactulose)
• Prevention and treatment of infections and bleeding
Etiological Treatment
• Discontinuation of the offending drug
• Treatment of viral hepatitis
• Abstinence from alcohol
Liver Transplantation
Liver transplantation is considered the definitive treatment for patients with advanced liver failure who do not respond to conservative management.
Conclusion
Liver failure is a complex medical condition that requires early diagnosis and prompt therapeutic intervention to reduce complications and improve survival outcomes. Advances in liver transplantation and intensive care management remain crucial in improving prognosis, along with preventive strategies targeting the underlying causes of the disease.
Lina Alaa Hussain
Al-Mustaqbal University
The First University in Iraq.