Scientific Article by Dr. Aseel Amer Hadi, Head of the Biochemistry Department Title: The Immunological Effects of the Human Immunodeficiency Virus and Their Role in the Development of AIDS
Scientific Article by Dr. Aseel Amer Hadi, Head of the Biochemistry Department
The Human Immunodeficiency Virus (HIV) is one of the most dangerous viruses affecting the human immune system. It leads to a gradual destruction of its vital functions, making the body vulnerable to opportunistic infections and malignant diseases. The advanced stage of HIV infection is known as Acquired Immunodeficiency Syndrome (AIDS), which represents the final phase of immune system failure. This article aims to highlight the immunological effects of HIV and their central role in the development of AIDS.
First: Mechanism of HIV Entry into Immune Cells
The Human Immunodeficiency Virus primarily targets immune cells carrying the CD4 receptor, notably Helper T cells (CD4+ T cells), in addition to Macrophages and Dendritic cells. The virus enters the cell by binding to the CD4 receptor and co-receptors such as CCR5 or CXCR4. It then fuses with the cell membrane and begins to replicate inside it, exploiting the host's cellular machinery.
Second: Immunological Effects of the Human Immunodeficiency Virus
HIV causes profound dysfunction in the immune system through several mechanisms, the most prominent of which are:
1. Destruction of Helper T Cells (CD4+): The continuous replication of the virus within these cells leads to their direct death or the induction of programmed cell death (apoptosis), causing a gradual decline in CD4 cell count. These cells are responsible for coordinating both cellular and humoral immune responses.
2. Impairment of Cellular Immune Response: As CD4 cell numbers decline, the immune system's ability to activate Cytotoxic T cells (CD8+) and Macrophages weakens, reducing the efficiency of eliminating pathogens.
3. Dysregulation of Humoral Immune Response: The virus affects the function of B cells, leading to abnormal antibody production, often without genuine effectiveness against the virus or other pathogens.
4. Chronic Immune Activation: The persistent presence of the virus leads to a state of chronic inflammation and immune activation, contributing to the exhaustion and accelerated deterioration of the immune system.
Third: The Role of Immunological Effects in the Development of AIDS
A severe decline in CD4 cell count (below 200 cells/mm³ of blood) is a key indicator of progression to the AIDS stage. At this stage, the immune system becomes incapable of defending the body, leading to the emergence of:
· Opportunistic Infections, such as Pneumocystis jirovecii pneumonia.
· Certain Cancers, such as Kaposi's sarcoma.
· Neurological Disorders resulting from central nervous system involvement.
These complications are not solely a direct result of the virus but stem from the near-complete collapse of immune function.
Fourth: The Impact of Antiretroviral Therapy on the Immune System
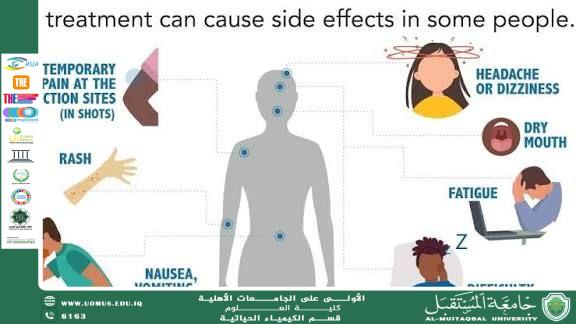
Antiretroviral Therapy (ART) has brought about a qualitative shift in controlling HIV. It works to reduce the viral load in the blood, allowing for a gradual increase in CD4 cell counts and improved immune function. Although the treatment does not completely eradicate the virus, it significantly delays the development of AIDS and reduces associated complications.
Al-Mustaqbal University – First among Iraqi Universities